睾丸旁胚胎性横纹肌肉瘤超声表现1例
2020-04-08 曹文斌 陈琴 吴昊 临床超声医学杂志
患者男,18岁,1年前左侧阴囊内发现一无痛性包块,初为拇指大小,进行性增大,现大小约8.0 cm×5.0 cm。超声检查:左侧阴囊内探及一大小约11.0 cm×4.0 cm&t
患者男,18岁,1年前左侧阴囊内发现一无痛性包块,初为拇指大小,进行性增大,现大小约8.0 cm×5.0 cm。超声检查:左侧阴囊内探及一大小约11.0 cm×4.0 cm×4.6 cm团状杂乱回声,边界不清,形态欠规则,未见正常附睾回声,左侧睾丸受压变形,位于团块中,与团块分界较清晰(图1)。
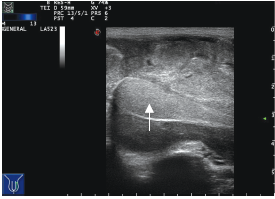
图1 声像图示左侧受压睾丸组织(箭头示)
超声造影:左侧阴囊内团状低回声早于右侧睾丸实质增强(与左侧受压睾丸实质同步增强),达峰时呈不均匀性高增强,增强后边界不清,大小未见明显变化,造影剂消退较慢(图2),考虑左侧附睾富血供肿瘤性病。
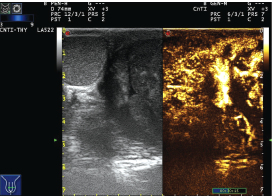
图2 超声造影呈不均匀性高增强
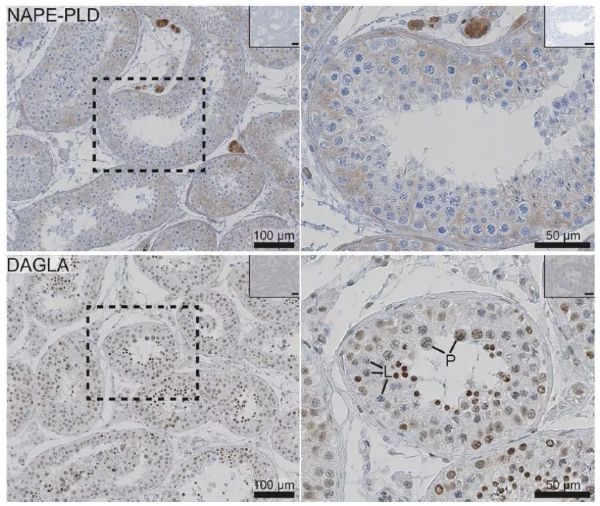
实验室检查:甲胎蛋白(AFP)1.03 ng/ml,人绒毛膜促性腺激素(HCG)1.02 U/L,前列腺特异性抗原0.93 ng/ml,人附睾蛋白40.5 ρmol/L。术中所见:左侧睾丸大小约11.0 cm×5.0 cm,与周围组织炎性粘连(图3)。术后免疫组化:desmin(+),Myogenin(+),α-SMA(+),Myoglobin(-),INI-1(+),病理证实:左侧睾丸旁胚胎性横纹肌肉瘤(图4)。

图3 左侧睾丸旁胚胎性横纹肌肉瘤术后大体标本(箭头示正常睾丸)
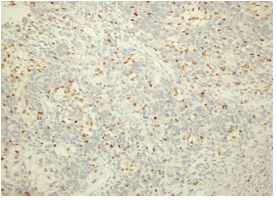
图4 左侧睾丸旁胚胎性横纹肌肉瘤病理图(HE染色,×200)
讨论:
横纹肌肉瘤是起源于横纹肌细胞或向横纹肌细胞分化的间叶性肿瘤,可分为胚胎性、腺泡状、多形性和梭形硬化性4个亚型。原发于附睾的横纹肌肉瘤极罕见,常表现为单侧阴囊内的无痛性包块,压迫神经时出现疼痛,较小时可能局限于睾丸旁组织,该病进展快,预后差,可有皮肤破溃或出血,早期确诊具有重要意义。血清肿瘤标记物HCG和AFP的测定对检查睾丸肿物有重要意义,几乎所有绒癌患者HCG 均有升高,在50%~90%非精原细胞瘤患者中有升高;AFP在75%以上非精原细胞瘤患者中有升高,本例患者AFP和HCG均正常。
发生于睾丸的胚胎性横纹肌肉瘤需与睾丸混合性生殖细胞肿瘤相鉴别,包括胚胎癌、卵黄囊瘤、恶性畸胎瘤、绒毛膜上皮癌等。本病例提示,对于短期内迅速增大的睾丸肿物,超声检查显示血流丰富且回声杂乱,超声造影表现为不均匀性高增强时,应考虑该病可能。
原始出处:
曹文斌,陈琴,吴昊,蔡志清.睾丸旁胚胎性横纹肌肉瘤超声表现1例[J].临床超声医学杂志,2019,21(01):12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#超声表现#
90
#胚胎#
72
#睾丸#
73
了解一下
147