JAMA Oncol:高强度放射或延缓前列腺癌扩散患者病情
2020-04-29 李羽壮 中国科学报
最近,美国研究人员在《美国医学会杂志—肿瘤学》上发表的一项研究报告称,高精度、高强度的立体定向消融放射(SABR)可能延缓部分已扩散到体内的前列腺癌患者病情。
最近,美国研究人员在《美国医学会杂志—肿瘤学》上发表的一项研究报告称,高精度、高强度的立体定向消融放射(SABR)可能延缓部分已扩散到体内的前列腺癌患者病情。
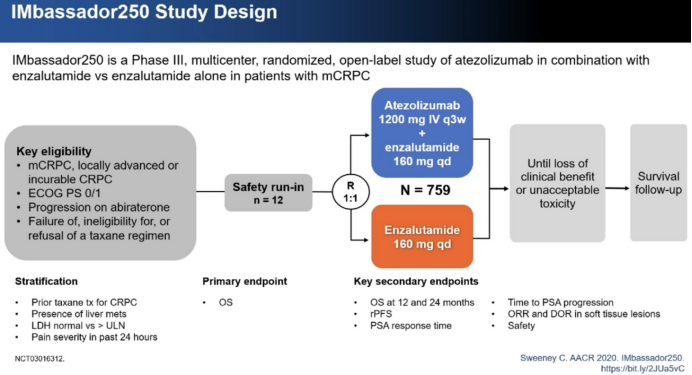
据悉,这项名为 ORIOLE 的试验(在寡转移性前列腺癌患者中对比观察法与立体定向消融放射治疗的 II 期随机试验的初步结果)自 2016 年在约翰斯 · 霍普金斯金梅尔癌症中心研究人员主导下开展,其目的是在寡转移性前列腺癌的复发病例中对比 SABR 与 “等待并观察” 法的疗效。
所谓的寡转移性癌是指已从原发肿瘤扩散到体内 1 到 3 个部位的肿瘤。据估计,在全球每年新诊断的 130 万前列腺癌患者中,约 20% 患有转移性疾病,但目前尚不清楚寡转移性癌患者的比例。
在美国,前列腺癌是第三大常见癌症,也是男性中最常见的癌症,每年导致约 3 万人死亡。转移性前列腺癌目前依然无法治愈,患有复发性激素敏感型癌症的男性,可能更愿意推迟其中一项标准治疗,也就是名为雄激素阻断治疗的抗激素疗法。因为该疗法会有勃起功能障碍、肌肉质量和体力下降、疲劳、体重增加和乳腺组织生长等副作用。
研究负责人、约翰斯 · 霍普金斯大学医学院放射肿瘤学和分子放射科学教授 Phuoc Tran 表示:“任何类型的放射,特别是 SABR,能否激发免疫系统反应一直都是一个有待解答的疑问,这个问题在免疫疗法盛行的当下尤显重要。我们的试验提供了迄今为止最好的数据,表明 SABR 可能引发全身免疫反应。”
在参加试验的 54 名男性中,接受 SABR 治疗的 36 名受试者中有 7 名(19%)在 6 个月内病情出现进展,而在仅接受观察的 18 名受试者中有 11 名(61%)病情出现进展。第六个月时新发癌症的风险也有所降低,接受 SABR 的受试者中有 16% 新发癌症,而在仅接受观察的受试者中这一比例为 63%。
研究发现,两组患者在有临床意义的副作用或报告与治疗相关的疼痛方面没有显着差异。参加 ORIOLE 试验的男性平均年龄为 68 岁,大多数受试者为白种人。
Tran 表示,对患者血液中免疫系统白细胞的分析表明,SABR 治疗与 T 细胞数量扩大有关,这意味着该治疗刺激了全身免疫系统对癌症产生反应。
研究结果表明,SABR 与其他免疫疗法相结合,对于治疗复发性寡转移性前列腺癌可能有效,但 Tran 提醒说,这种联合疗法的任何潜在益处都需要在未来的临床试验中进行检验。
Tran 说,SABR 治疗可能会去除或影响在复发性寡转移性前列腺癌中促使微转移进展的信号,而不仅仅是 “重置疾病的时钟” 直至转移灶再次变大。
未来,该团队将继续开展 II 期研究,以确定是否可以增加疾病进展较慢的受试者数量。
原始出处:
Michael J. Raphael, et al. Factors Associated With Chemoradiation Therapy Interruption and Noncompletion Among Patients With Squamous Cell Anal Carcinoma. JAMA Oncol. Published online April 23, 2020. doi:10.1001/jamaoncol.2020.0809.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
58
#病情#
68
#高强度#
63
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
82
谢谢梅斯分享这么多精彩信息
75
前列腺癌相关研究,学习了,谢谢梅斯
70