手术治疗局部晚期原发性胸腺腺癌一例
2019-05-20 赵凯 夏宗江 王旭广 郑州大学学报(医学版)
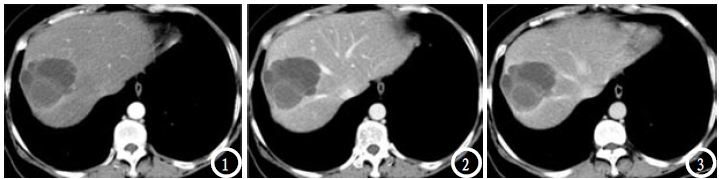
患者, 38 岁,女,就诊前 3 个月,自 觉晨起眼睑浮肿,日间正常,未在意; 随后眼睑水肿 持续时间变长,同时出现脸部水肿,颈部血管充盈扩 张;情绪激动时加重,夜间平卧逐渐受限。入院前 1 周,脸浮肿加重,出现胸部紧缩感,胸背部疼痛等症 状;无眼睑下垂、咀嚼无力、吞咽困难、乏力等重症肌 无力症状;体格检查无特殊异常,既往体健。胸部增 强 CT 发现前纵隔有一约52 mm ×49 mm 大小软组

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
89
#胸腺#
75
#局部晚期#
91
#胸腺腺癌#
70
#手术治疗#
81
#局部#
69