众所周知,桡骨远端骨折常合并下尺桡关节(distal radioulnar joint,DRUJ)损伤。未能认识并适当治疗这些伴随的损伤,可能会导致腕部的功能障碍。
DRUJ是一个复杂的解剖单位,在桡骨远端和尺骨之间提供关节连接。它由骨和软组织结构组成,与上桡尺关节一起,允许前臂进行旋转(旋前/旋后)。理解DRUJ的解剖结构,对治疗桡骨远端骨折及避免并发症至关重要。
注:本文为最新文献翻译(Nypaver C, Bozentka DJ. Distal Radius Fracture and the Distal Radioulnar Joint. Hand Clin. 2021 May;37(2):293-307. doi: 10.1016/j.hcl.2021.02.011. )。原文较长,本贴为前半部分内容。
一、解剖
-
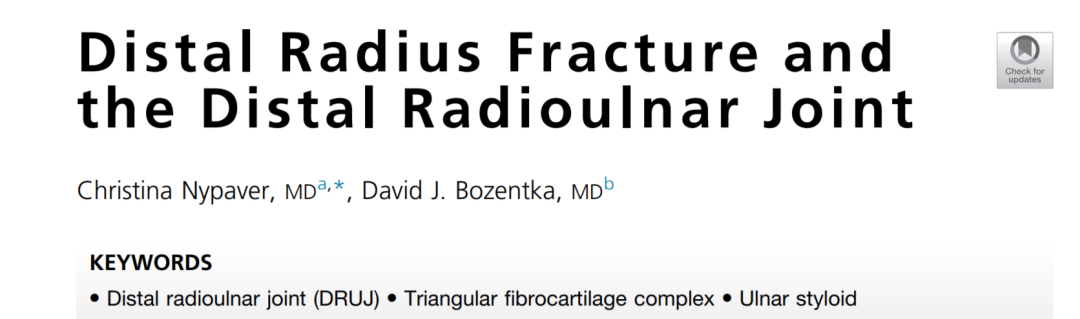
尺骨是前臂的稳定部分,它的远端头包括一个关节面,桡骨通过已状切迹绕着它旋转。
-
桡骨乙状切迹的曲率半径大于尺骨关节面的曲率半径,这允许半径在150°和180°之间旋转(图1)。
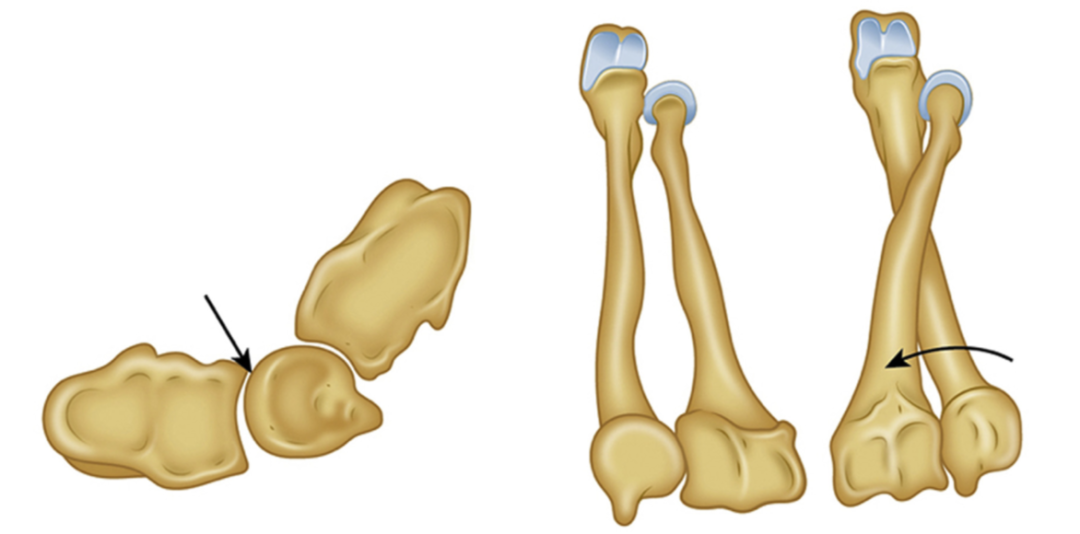
图1:下尺桡关节的活动。
-
乙状切迹的背侧和掌侧边缘有助于关节稳定。然而,骨性解剖结构是可变的,并且本质上是不稳定的。因此,DRUJ的软组织结构对于稳定至关重要。
-
尺骨头与三角形纤维软骨复合体(TFCC)相连,后者是DRUJ最重要的软组织稳定部分。
-
尺骨茎突是尺骨远端的骨性突起,在其底部是一个浅凹,称为中央凹,是软组织附着的关键区域。
-
尺骨远端及其相对于桡骨远端的长度因人而异,这被称为尺骨变异——尺骨比桡骨长被称为正变异,而尺骨比桡骨短被称为负变异。
-
尺腕骨关节的负荷传递随着正变异而增加,这也尺骨撞击的可能性,其中远端尺骨病理性地撞击腕骨。 -
尺骨变异可以在标准的后前位透视片上测量,手腕处于中立位。(通过桡骨远端关节面画一横线,垂直于其纵轴,这条线和尺骨穹窿远端边缘之间的距离(图2)。

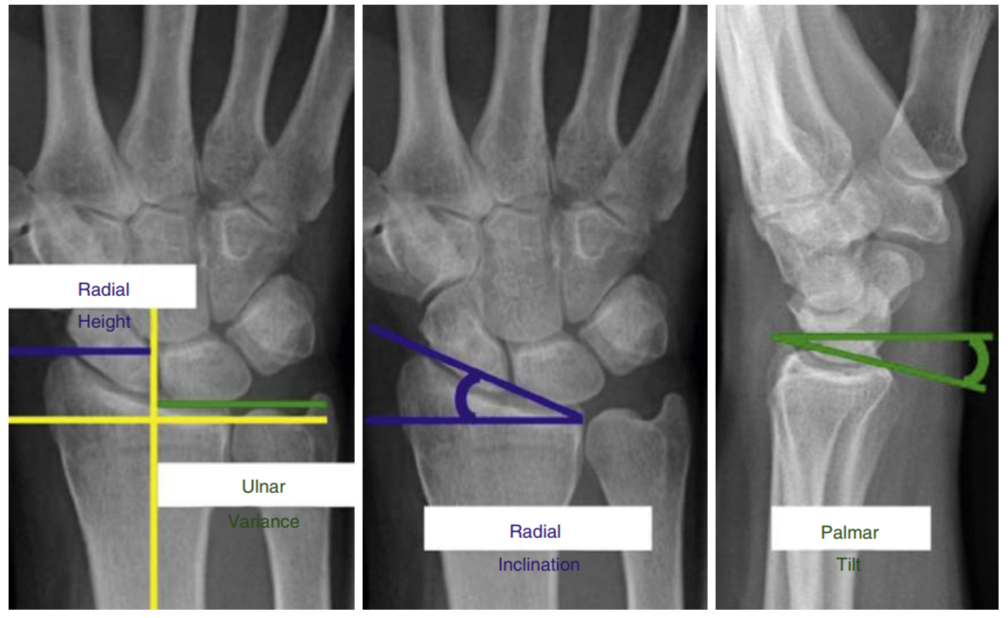
图2:尺骨变异的测量方法。自桡骨远端关节面与尺骨远端关节面间的距离。
2. DRUJ软组织解剖要点(Review of Soft Tissue Distal Radioulnar Joint Anatomy)
-
TFCC由三角纤维软骨及支持下尺桡关节和尺腕关节的韧带结构组成。
-
TFCC的桡尺关节掌侧韧带和背侧韧带对DRUJ的稳定至关重要。
-
它们起源于乙状切迹的背侧和掌侧边缘,在冠状面上分为浅(远)和深(近)支。
-
浅支附着于尺骨茎突的基底部和中部,而深支附着于中央凹(图3)。

图3:桡尺关节掌侧与背侧韧带。
-
深支赋予DRUJ高度稳定性——考虑到桡骨远端骨折,尤其是尺骨茎突骨折对DRUJ的损伤,其解剖位置在临床上变得很重要。
-
尺骨远端(相对于桡骨)背侧平移的主要限制是桡尺掌侧韧带,而桡尺背侧韧带阻止尺骨远端掌侧平移。
-
TFCC的三角形纤维软骨本身(或关节盘)作为关节面吸收来自腕骨的压缩负荷。
-
DRUJ的其他软组织稳定器包括旋前方肌、尺侧腕伸肌腱、DRUJ关节囊和骨间膜,特别是骨间膜的远端斜束,其存在于大部分人群中。
二、背景
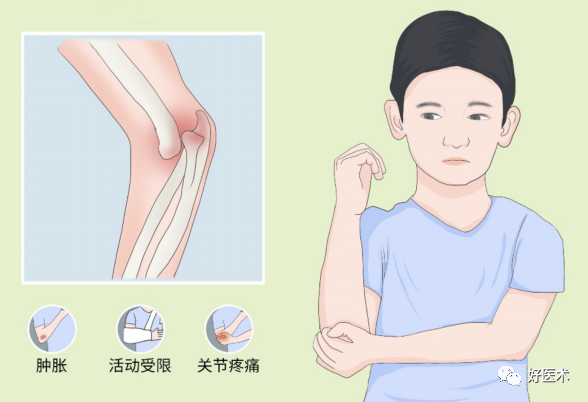
约2%-37%的桡骨远端骨折患者在骨折愈合后出现DRUJ不稳定,约三分之二的患者出现活动范围缩小和腕尺侧疼痛的症状。
DRUJ的损伤可以是骨损伤、软组织损伤或两者兼而有之。预测这些损伤是否导致临床相关或有症状的DRUJ不稳定/不协调仍在文献中进行评估。
三、下尺桡关节损伤的临床相关性与发生率
许多研究评估了桡骨远端骨折的特点及其在DRUJ不稳定或不协调中的作用。
Naka-mura和colleaguesshowed指出,桡侧移位和尺偏角的丢失是TFCC桡尺侧韧带中心凹撕脱的重要预测因素。Dy和collegues证明,在具有明显骨间膜远端斜束的尸体标本中,2mm的冠状移位增加了背-掌侧DRUJ移位。
桡骨短缩也与DRUJ问题风险增加相关。
桡骨远端骨折伴有关节内延伸至乙状切迹的情况发生在约55%的背侧成角关节内骨折中,这在计算机断层扫描(CT)上可能更容易识别(图4)。
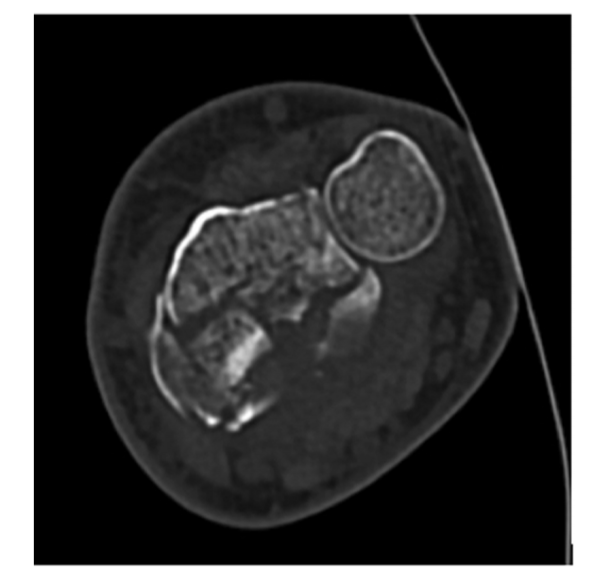
图4:CT横断面可见桡骨远端骨折累及乙状切迹。
任何骨折的关节内延伸导致的明显问题是关节面的解剖不协调,这最终会导致退行性改变和关节炎。
尽管桡骨远端骨折关节内2mm的台阶被广泛接受为骨折后几乎肯定会发生关节炎的临界值,但这项研究的大部分涉及关节内延伸到桡腕关节,而不是DRUJ。
Vitale和同事评估了骨折延伸到乙状切迹的患者,发现这些患者在接受手术治疗时,并没有更高的DRUJ关节炎发生,并且根据DASH评分的差异,只有冠状面偏离大于1mm的骨折才有更高水平的上肢功能障碍。
关节内伸展也可能在DRUJ不稳定的发展中起作用。Bombac和其同事发现,当骨折线延伸到乙状切迹并伴有尺骨茎突骨折时,相关的TFCC发生率更高。损伤比其他桡骨远端骨折类型更严重。
乙状切迹掌侧或背侧缘移位性骨折可能导致关节提供的骨稳定性丧失,导致DRUJ不稳定。
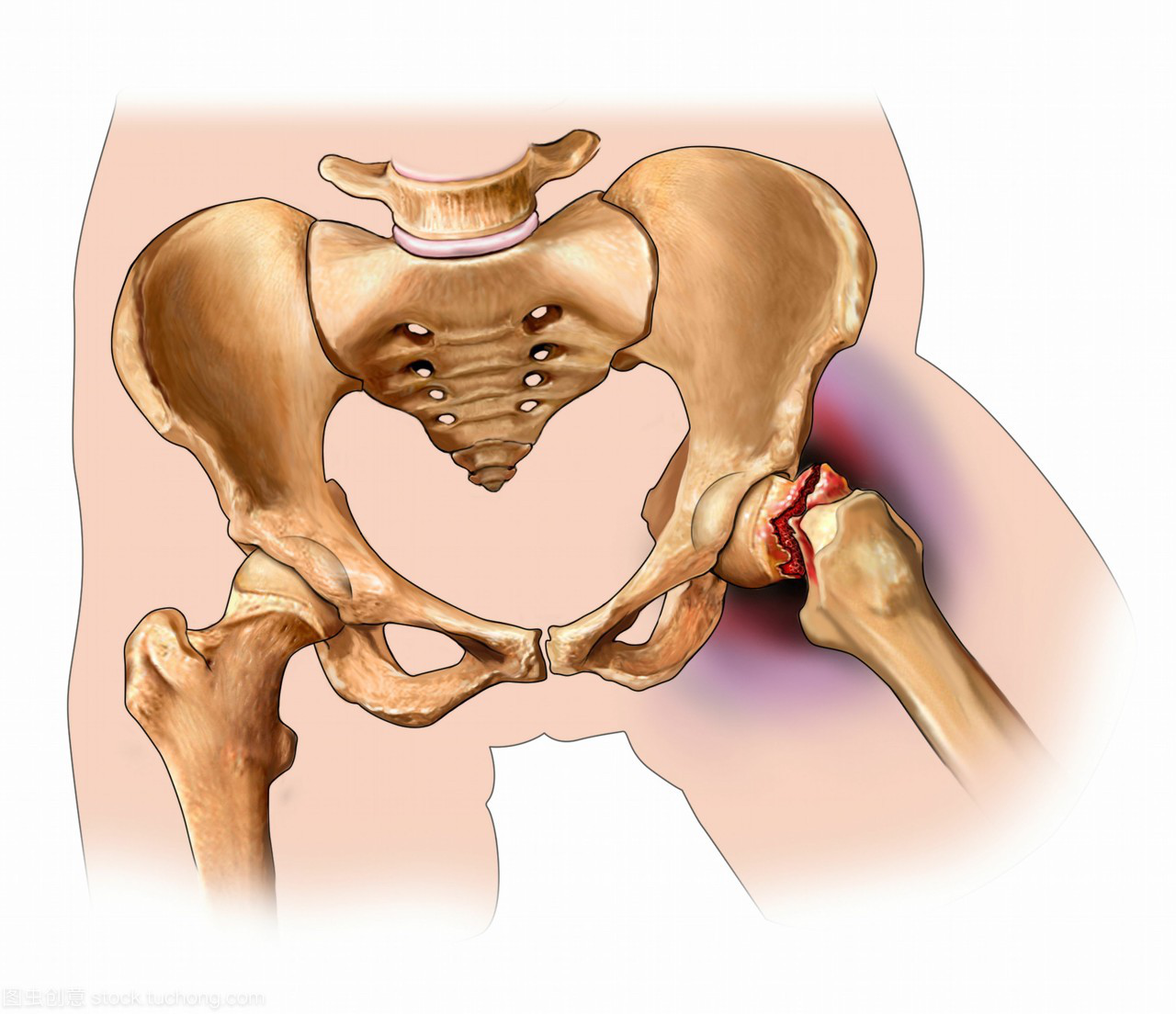
3. 尺骨茎突骨折

图5:桡骨远端骨折合并尺骨茎突骨折。
类似地,尺骨茎突骨折移位超过2mm被报道与DRUJ不稳定有关。
然而,许多研究表明,在手术治疗的桡骨远端骨折中,没有可识别的DRUJ不稳定性证据,无论骨折移位或位置如何,尺骨茎突骨折的存在不影响功能结果。可能的解释是尺骨茎突骨折在桡骨远端骨折固定后移位较少,或者有其他保持完整并保持DRUJ稳定性和一致性的DRUJ软组织稳定结构。
尽管一些研究人员认为尺骨茎突骨折不愈合与DRUJ的不稳定性和“不太有利”的结果有关,但其他研究人员已经证明它与疼痛、不稳及桡骨远端骨折术后功能减退无关。
TFCC三角纤维软骨复合体撕裂是桡骨远端骨折最常见的相关损伤,发生在高达84%的骨折中。许多研究者评估了TFCC撕裂和DRUJ不稳定性之间的联系,特别是外周TFCC撕裂,这是桡骨远端骨折中最常见的撕裂部位。
Kwon和其同事确定,他们研究中所有DRUJ不稳定的患者都有来自尺骨头凹或乙状切迹的深TFCC撕脱性撕裂。这些发现与Lindau及其同事的发现相似,他们发现11名经关节镜证实的完全性外周TFCC撕裂患者中有10名在随访评估时具有DRUJ不稳定性。
其他研究人员认为TFCC的外周部分血管丰富,因此具有良好的愈合潜力,只要韧带接近并且患者被固定一段时间以允许愈合。需要注意的是,外周关节盘的血管供应确实随着年龄的增长而减少。
四、评价、评估与影像(急性损伤)
-
初次就诊时,良好的病史和体检是必须的。
-
开放性伤口可能意味着更高的能量机制,因此对DRUJ损伤的可能性增加。
-
评估DRUJ损伤的一个关键步骤是获得腕部的平片,包括真实的侧位片和有关节内受累时的CT扫描。
-
影像学应允许评估桡骨远端和尺骨远端骨折特征,这些特征可能与DRUJ损伤有关(见三角形纤维软骨复合体撕裂和图6)。

图6:桡骨远端骨折闭合复位后,可见下尺桡关节距离增宽,尺骨正向变异。考虑DRUJ损伤。
-
影像学检查还可以识别正的尺骨变异、DRUJ变宽或尺骨相对于桡骨的半脱位/脱位。
-
6mm或更大的尺骨正向变异和1mm的DRUJ增宽会增加DRUJ不稳定的风险。
-
TFCC的裂伤可以通过核磁共振或关节镜来诊断,这是标准。
-
没有足够的证据支持对所有急性桡骨远端骨折进行磁共振成像。
-
急性情况下需要干预的TFCC撕裂通常在术中处理。
-
使用这些线索可以帮助手外科医生提高他们对DRUJ可能受伤的怀疑。然而,大多数研究者会同意,根据本文其他地方讨论的文献,对DRUJ的临床评估应该在桡骨远端解剖复位后进行,因为这一步骤本身可以恢复DRUJ的稳定性和一致性。大多数人也同意这种临床评估应该与对侧进行比较,因为患者之间可能存在韧带变异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









客观分析。彻底明了。
137
#桡关节#
118
#损伤#
111
#桡骨远端骨折#
128
#桡骨#
87
谢谢分享
102