Clin Cancer Res:多发性骨髓瘤:来那度胺的“大剂量”累觉不爱
2020-11-17 MedSci原创 MedSci原创
对于多发性骨髓瘤,大剂量化疗和自体造血干细胞移植(ASCT)继以来那度胺(10-15 mg/天)维持治疗(LenMT)被认为是标准疗法。然而,根据不良反应而降低剂量常有发生,随时间推移而达到的LenM
对于多发性骨髓瘤,大剂量化疗和自体造血干细胞移植(ASCT)继以来那度胺(10-15 mg/天)维持治疗(LenMT)被认为是标准疗法。然而,根据不良反应而降低剂量常有发生,随时间推移而达到的LenMT剂量中位水平可能更低。迄今为止,LenMT期间的剂量反应尚未被研究过。
这是一项多中心、随机、开放标签的临床试验,ASCT和大剂量来那度胺(25 mg/天)巩固治疗(CT)后的多发性骨髓瘤患者被随机分至LenMT 25 mg/天组或5 mg/天组。主要终点是无进展存活期(PFS)。
研究流程
两组各有94位患者(中位年龄58岁),其中22%的患者为国际分期系统(ISS)3期,22%的患者处于晚期缓解中(CR)。
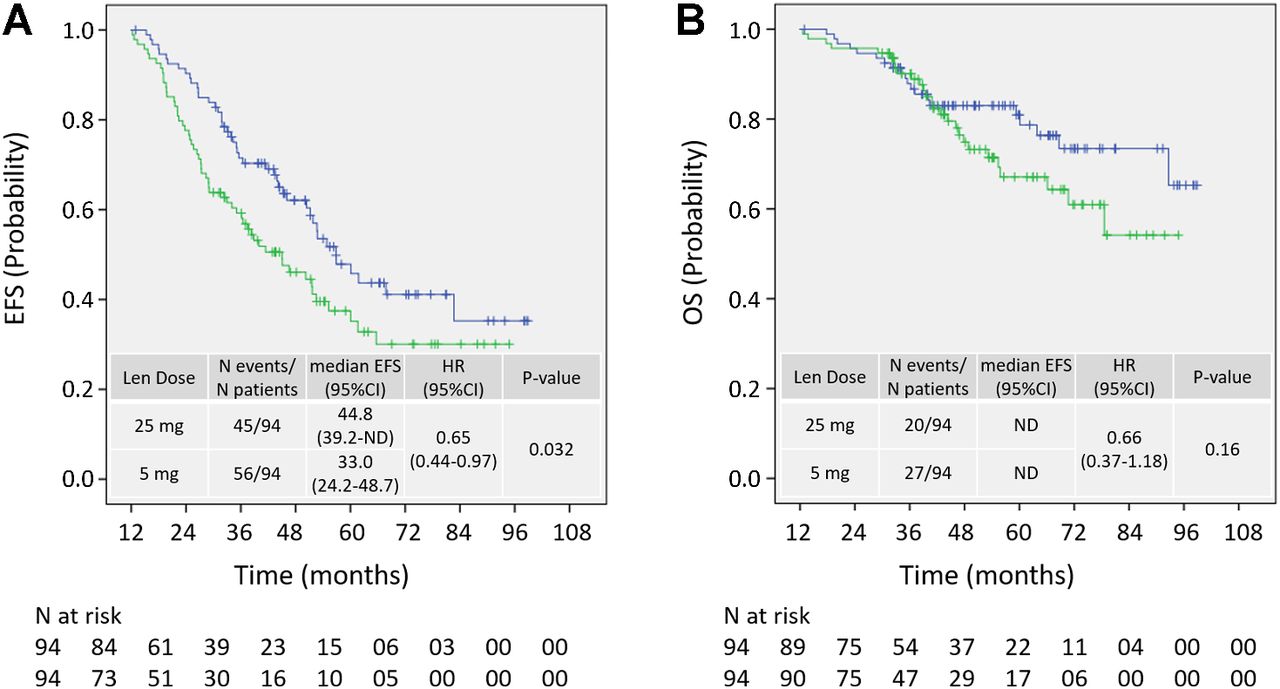
25 mg组(蓝色)和5 mg组(绿色)随机分组后的PFS和OS
经过中位随访46.7个月,两组的中位剂量分别为14.5和5 mg/天;53%的减剂量都发生于CT期间。大剂量组和低剂量组的中位PFS分别是44.8个月和33.0个月(HR 0.65; 95% CI, 0.44–0.97; P=0.032),36%和23%的患者获得严格的完全缓解(最佳缓解),4年OS分别是79%和67%(P=0.016)。血液性毒性、≥3级中性粒细胞减少症和感染都多见于LenMT 25 mg用药,且均随着剂量的调整而减少。
总之,LenMT剂量与疗效和毒性相关。在巩固治疗期间减剂量的高概率提示或许不应该采用高初始剂量。
原始出处:
Roland Fenk, et al. Efficacy and Tolerability of High- versus Low-dose Lenalidomide Maintenance Therapy of Multiple Myeloma after Autologous Blood Stem Cell Transplantation. Clin Cancer Res November 15 2020 26 (22) 5879-5886; DOI:10.1158/1078-0432.CCR-20-0841
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
73
受教了
153
#大剂量#
88
挺好的
131
受益匪浅
102
不错
152