JACC:LPA KIV-2突变降低了脂蛋白(a)的浓度并降低冠状动脉疾病的发生
2021-07-31 MedSci原创 MedSci原创
LPA KIV-2区域的功能突变决定了Lp(a)的变异和CAD风险。即使是适度但终生的遗传性Lp(a)降低也会转化为明显的CAD风险降低。
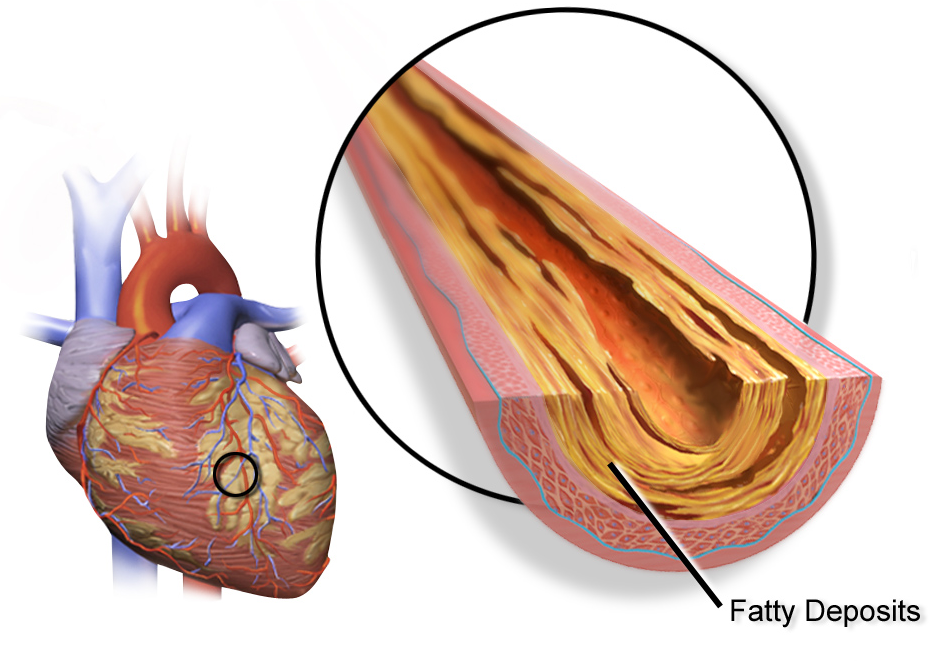
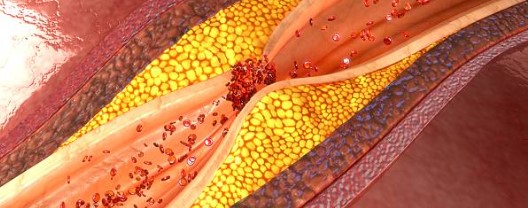
脂蛋白(a)(Lp(a))性状是一个重大谜题。Lp(a)具有多种促炎、促动脉粥样硬化和潜在的促血栓形成的特性,并与心血管疾病(CVD)有关,包括冠状动脉疾病(CAD)、心力衰竭、主动脉瓣狭窄、周围动脉疾病、中风、心血管疾病和总死亡率。
在普通人群中,Lp(a)的浓度呈现出1000倍的浓度范围,不同种族之间的中位浓度相差近10倍,甚至在欧洲内部也有2至3倍的差异。与其他显示高度多基因遗传结构的脂蛋白不同,超过90%的Lp(a)变异由一个基因控制,即编码脂蛋白(a)(apo(a))的LPA基因。
LPA的基因结构很复杂,大部分的编码序列不能被常规的测序或基因分型技术所获得。LPA有一个高度重复的结构,由10个高度同源的kringle IV(KIV)结构域(亚型1至10)、一个kringle V结构域和一个蛋白酶结构域组成。
有趣的是,虽然1个低分子量等位基因通常足以导致Lp(a)浓度的增加,但具有相同等位基因组合的两个人的Lp(a)浓度仍然可以相差200倍。事实上,几乎在每一个同种异构体组中都能发现Lp(a)值非常高或非常低的个体。这意味着除了KIV大小的多态性外,还存在对Lp(a)浓度有很大影响的其他遗传变异。
高达70%的LPA编码序列位于高变异的kringle IV型(KIV-2)区域。传统的技术很难进入该区域,但可能包含功能变异。为此,来自因斯布鲁克医科大学遗传流行病学研究所试图研究新的、非常频繁的剪接变体KIV-2 4733G>A对Lp(a)和CAD的影响,结果发表在JACC杂志上。
研究人员在GCKD(德国慢性肾脏病)研究中(n = 4673)通过等位基因特异性PCR对4733G>A进行了基因分型,进行了迷你基因检测,确定了代理单核苷酸多态性,并通过英国生物库(n = 440234)的生存分析来描述其对CAD的影响。在1000个基因组项目中评估了种族群体的频率。
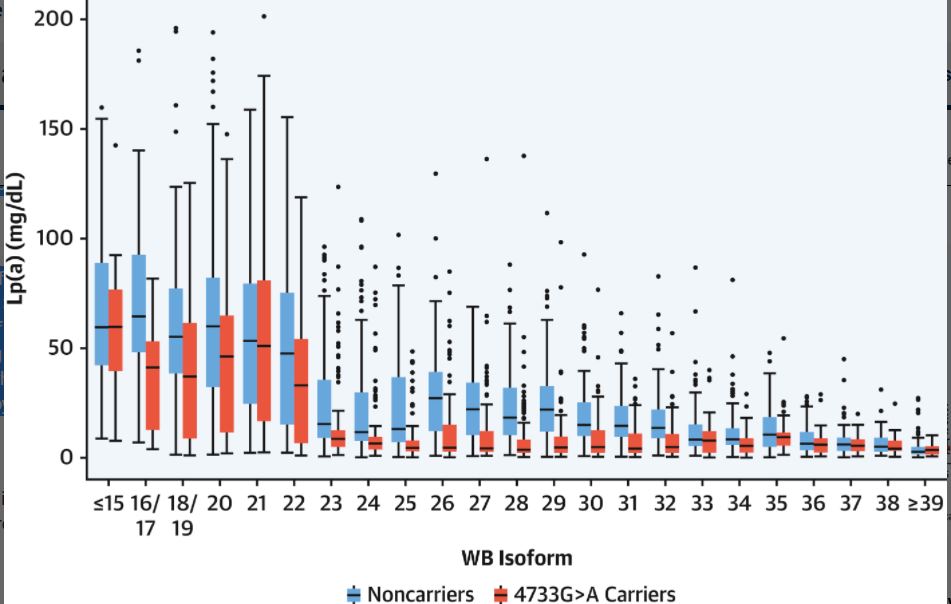
GCKD中按载体状态和异构体1分类的Lp(a)浓度
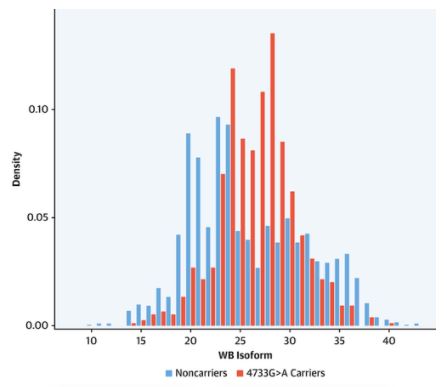
结果显示,4733G>A变体(38.2%的携带者频率)在大多数等位基因大小中被发现。它减少了等位基因的表达,但没有废除蛋白质的产生,使Lp(a)降低了13.6 mg/dL(95% CI: 12.5-14.7),同时是继小异构体之后最强的方差解释因素。
4733G>A和4925G>A(另一个KIV-2剪接突变)的复合杂合占人口的4.6%。与野生型相比,Lp(a)降低了31.8mg/dL,最重要的是将四分位数范围缩小了9倍(从42.1到4.6mg/dL)。在英国生物库中,4733G>A单独和与4925G>A的复合杂合使CAD的HR降低9%(95%CI:7%-11%)和12%(95%CI:7%-16%)。
GCKD中4733G>A携带者状态的同种异体1的分布情况
综上,LPA KIV-2区域的功能突变决定了Lp(a)的变异和CAD风险。即使是适度但终生的遗传性Lp(a)降低也会转化为明显的CAD风险降低。
参考文献:
Frequent LPA KIV-2 Variants Lower Lipoprotein(a) Concentrations and Protect Against Coronary Artery Disease. J Am Coll Cardiol. 2021 Aug, 78 (5) 437–449
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
49
#冠状动脉疾病#
64
#ACC#
61
#脂蛋白#
46
#浓度#
52
#LPA#
74