高危胸痛,明确诊断要快
2016-08-29 陈都 苏州大学附属第一医院急诊科 医学界急诊与重症频道
反复胸骨后疼痛三天患者男性,39岁,因“反复胸骨后疼痛三天,再发并加重一小时”由 120 送入我院。发病时患者无咯血,无晕厥,疼痛间断有缓解,但发作时表情异常痛苦伴大汗。患者血压 115/75 mmHg,心率 55 次/分,脉氧 100%,体温 36.5 度,表情痛苦,心肺听诊未及明显异常。床边检查:心电图提示窦性心动过缓;血气分析提示血钾 2.5 mmol/L,乳酸 4.3 mmol/L,PH
反复胸骨后疼痛三天
患者男性,39岁,因“反复胸骨后疼痛三天,再发并加重一小时”由 120 送入我院。发病时患者无咯血,无晕厥,疼痛间断有缓解,但发作时表情异常痛苦伴大汗。
患者血压 115/75 mmHg,心率 55 次/分,脉氧 100%,体温 36.5 度,表情痛苦,心肺听诊未及明显异常。床边检查:心电图提示窦性心动过缓;血气分析提示血钾 2.5 mmol/L,乳酸 4.3 mmol/L,PH 值、氧分压及二氧化碳分压正常,立即给予静脉输液、补钾补镁。
向家属交代病情,告知病情危重,属高危胸痛,随时可能猝死,胸痛原因需进一步检查。
相关检查陆续回报:心肌酶谱及肌钙蛋白正常;血常规提示白细胞 15.3 ×109 /L;平扫 CT 及大血管 CTA 临时报告未见主动脉夹层、肺栓塞、气胸、肺部感染迹象,也未报食道异物。
诊断思路
急诊遇到胸痛患者首先应该排除高危胸痛:如心梗、主动脉夹层、肺栓塞。结合病史、疼痛特点、心电图等资料,上述三者缺乏证据,亦不能解释患者的临床表现。但患者疼痛时大汗淋漓伴重度低钾,提示病情危重,应属于高危胸痛患者,必须尽快明确诊断。
请胸外科会诊
进一步研读 CT 片,在电脑上调取薄层 CT 影像时发现有几个层面患者食道中可见不规则突起(图1),考虑食道异物。
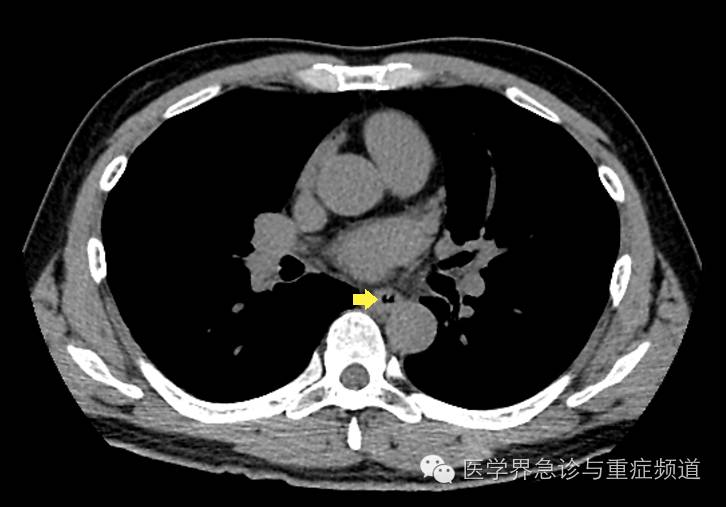
图1 . 胸部CT扫描可见食管内壁不规则突起
追问病史,不能停留在影像上
患者近期有吃鱼史,自诉进食过程中似有食道异物感,但未予重视,随后几天游泳过程中症状逐渐加重,就诊当日再次发作且不能忍受,呼叫 120 送入我院急诊。
为此,我们再次和影像科医生沟通,影像科值班医生认为食道内像软组织影,不像鱼刺。但如果不是卡鱼刺,患者临床症状很难解释,我们认为根据临床表现还是应该高度怀疑卡鱼刺。
由于诊断不明确,消化科值班医生也不敢贸然行急诊内镜检查。
为了明确诊断,进一步对患者行食管碘剂棉透视检查可见食管中段碘剂棉絮挂钩现象(图2),符合食道异物表现。我们请影像科资深专家结合病史再次读片,专家认为薄层 CT 可见食道内壁异物,纵隔可见少量积气,大血管未见异常,结合患者疼痛特点和血常规表现考虑食道异物并发食道穿孔感染,遂行食管内镜异物取出术,收入病房进一步治疗。
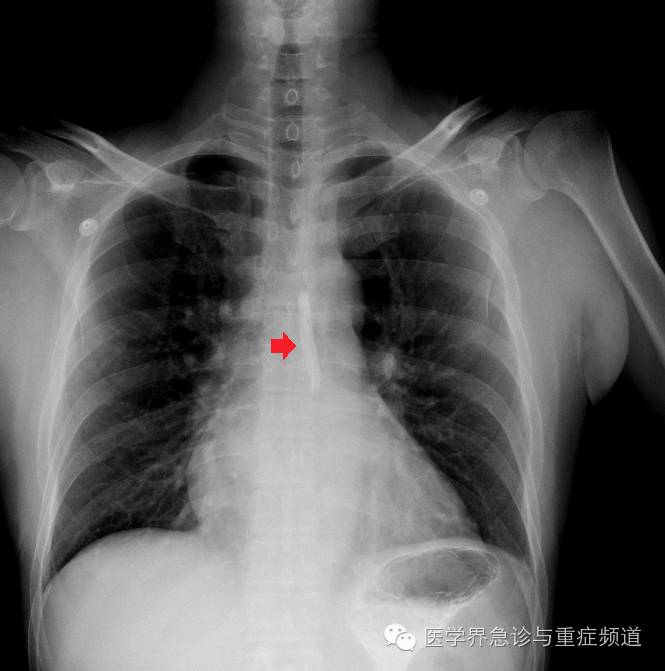
图2 . 食管碘剂棉透视可见食管中段挂钩现象
思考总结
1. 高危胸痛除了心梗、主动脉夹层、肺栓塞,要考虑到食道异物可能。回头再看这个患者,其阵发性胸痛可以用食道的节律性蠕动解释,白细胞升高可以用感染解释,可见一元论、反证法有时可帮助我们确立诊断假设。
2. 不要过度依赖影像医生的初步诊断,临床医生再次读片很有必要,遇到诊治困难时应该请专家介入,及时明确诊断,以免延误治疗。
3. 病史对影像诊断尤为重要,不能只停留在影像上。
4. 急诊遇到诊断不明患者,首要任务是病情评估,关注生命体征,在第一时间和患者及家属沟通疾病风险并告知诊疗计划,以便赢得患者及家属的理解和配合。其次,在对症治疗的同时有针对性的完善相关检查,尽早明确诊断。必要时应果断请相关科室会诊,弥补个人临床思维和专业知识局限。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习啦
90
很实用,谢谢
0
继续学习
77
继续关注
77