JCEM:甲状腺乳头状癌复发危险因素的全面评估
2021-11-21 MedSci原创 MedSci原创
研究人员新提出的基于组合mRNA和microRNA表达的风险模型可作为复发的预后指标,这些结果有助于更早地预测复发。
甲状腺癌复发与死亡率增加有关,并且甲状腺癌复发的早期检测已被证明可以改善患者的预后。目前使用临床工具预测复发风险,这些工具通常在癌症治疗后对患者进行再分期。虽然这有助于根据术后随访水平和TSH抑制程度对患者进行分层,但它不会告知外科医生和患者复发风险。因此,需要详细了解疾病发作时的复发风险可能会使患者得带个性化和改进的治疗。

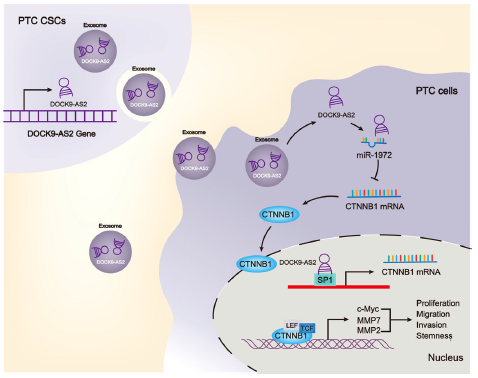
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在对复发性肿瘤中明显的3个水平的遗传变化(mRNA、microRNA和体细胞突变)进行全面的生物信息学和实验分析,并构建新的组合预后风险模型。
研究人员分析了癌症基因组图谱数据(TCGA),以确定46例复发性和455例非复发性甲状腺肿瘤中的差异表达基因(mRNA/microRNA)。两个外显子突变分析用于鉴定体细胞突变。功能基因分析是在多种甲状腺细胞系的细胞分析中进行的。研究人员使用TCGA数据集评估基因的预后价值。
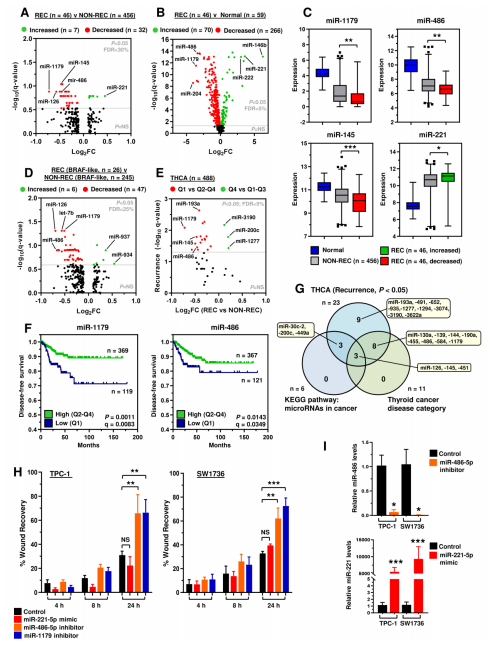
研究人员共确定了128个与复发相关的新的潜在生物标志物,包括40个mRNA、39个miRNA和59个遗传变异。在差异表达基因中,FN1、ITGα3和MET的调节对甲状腺癌细胞迁移有显著影响。类似地,miR-486和miR-1179的消融显著增加了TPC-1和SW1736细胞的迁移能力。研究人员进一步利用具有经过验证的功能作用基因,并确定了5个基因风险评分分类器作为甲状腺癌复发的独立预测因子。
由此可见,研究人员新提出的基于组合mRNA和microRNA表达的风险模型可作为复发的预后指标,这些结果有助于更早地预测复发。
原始出处:
Hannah R Nieto,et al.Recurrence of Papillary Thyroid Cancer: A Systematic Appraisal of Risk Factors.JCEM.2021.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgab836/6429719
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCEM#
109
#乳头状#
100
#JCE#
81
。。。
107
学习了#肿瘤#
118
#甲状腺乳头状癌#
83
混积分
114