Heart:冠脉造影与心衰的预后有关?
2017-08-14 nanchao.H MedSci原创
对于较严重的心衰患者,往往会行冠脉造影术,然而,心衰患者冠状动脉造影术的决定因素和相关临床结果知之甚少。 本研究(BIOSTAT-CHF)纳入了2516名有明显临床症状的心衰患者,包括住院治疗的病人和院外治疗的患者。研究结果显示,有315名(12.5%)心衰患者在出现了明显临床症状后30天内接受了冠脉造影术。在接受了冠脉造影的患者中,大多数是住院病人,伴有较明显的急性冠脉综合征,肌钙蛋白I的
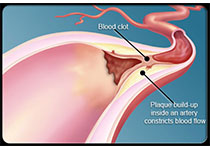
对于较严重的心衰患者,往往会行冠脉造影术,然而,心衰患者冠状动脉造影术的决定因素和相关临床结果知之甚少。
本研究(BIOSTAT-CHF)纳入了2516名有明显临床症状的心衰患者,包括住院治疗的病人和院外治疗的患者。研究结果显示,有315名(12.5%)心衰患者在出现了明显临床症状后30天内接受了冠脉造影术。在接受了冠脉造影的患者中,大多数是住院病人,伴有较明显的急性冠脉综合征,肌钙蛋白I的水平也较高,更年轻,并且肾功能相对更好(所有的p≤0.01)。另外,接受了冠脉造影的患者的心衰住院风险更低(HR=0.71, 95% CI 0.57-0.89, p=0.003),死亡率也更低(HR=0.59, 95% CI 0.43-0.80, p=0.001)。在行冠脉造影术的患者中,伴有冠脉狭窄的患者(39%)的临床预后要更差(HR =1.71, 95% CI 1.10-2.64, p=0.016)。
研究结果表明,在有明显症状的心衰患者中,仅有<13%的患者接受了冠脉造影术。相比于没有接受冠脉造影的患者,接受了冠脉造影术患者的不良预后结局发生风险要明显降低。
原始出处:
Joao P et al.Coronary angiography in worsening heart failure: determinants, findings and prognostic implications.Heart.2017 Aug.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ART#
58
#冠脉造影#
88
#造影#
66
#HEART#
79
学习一下
100