Lancet neurol:院前溶栓的移动卒中治疗单元优于传统治疗吗?
2016-07-16 MedSci MedSci原创
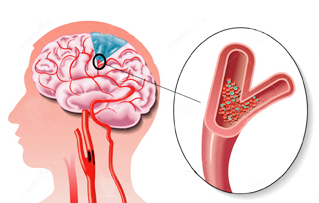
配备特殊CT设备的移动卒中治疗单元,可在入院前对患者进行溶栓治疗,缩短了急性缺血性卒中患者静脉溶栓的时间;然而,院前溶栓对临床预后的直接效果还不明确。我们比较了急性缺血性卒中患者接受急诊移动治疗单元或传统治疗的3个月功能预后。 在这个观察性登记研究中,急性缺血性卒中患者经由急救车使用卒中急诊移动单元(STEMO)(院前治疗覆盖了130万柏林居民)接受溶栓治疗(阿替普酶)或使用传统治疗(普通救
配备特殊CT设备的移动卒中治疗单元,可在入院前对患者进行溶栓治疗,缩短了急性缺血性卒中患者静脉溶栓的时间;然而,院前溶栓对临床预后的直接效果还不明确。我们比较了急性缺血性卒中患者接受急诊移动治疗单元或传统治疗的3个月功能预后。
在这个观察性登记研究中,急性缺血性卒中患者经由急救车使用卒中急诊移动单元(STEMO)(院前治疗覆盖了130万柏林居民)接受溶栓治疗(阿替普酶)或使用传统治疗(普通救护车,在柏林本杰明富兰克林慈善大学接受治疗)。记录STEMO(院前)或传统治疗(住院期间)的患者的治疗数据,结局和人口统计资料。主要终点是出院在家下次卒中前不需要接受帮助的患者比例,以及3个月时改良Rankin量表(mRS)评分为1分或更低。校正人口统计学,并发症和卒中严重程度进行多变量逻辑回归分析。
结果:在2011年2月5日到2015年5月5日,427例患者接受STEMO治疗,505例患者接收传统治疗。STEMO组305例患者符合入组条件,传统治疗组353例符合。STEMO组161人(53%)患者VS 传统治疗组166人(47%)mRS评分小于1分或更低(p=0.14)。与传统治疗组相比,STEMO组主要终点(OR 1·40, 95% CI 1·00–1·97; p=0·052) 的调整风险比 (ORs)差异不显著。
结果表明,STEMO组与传统治疗组相比mRS小于1或更低评分无显著差异。然而,我们的结果显示了院前开始静脉溶栓可能会提高患者的功能预后。这需要更大规模的试验来证实。
原始出处:
Dr Alexander Kunz, MDcorrespondenceemail, Martin Ebinger, MD, Frederik Geisler,et al,Functional outcomes of pre-hospital thrombolysis in a mobile stroke treatment unit compared with conventional care: an observational registry study,lancet neurol ,15 July 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Lancet#
62
#Neurol#
74
#院前#
65
好文值得点赞!继续关注学习。
85