PLoS One:发现一种可遏制癌细胞转移的基因
2015-02-17 新华 新华网
日本名古屋市立大学的一个研究小组在新一期的美国在线科学杂志《公共科学图书馆综合卷》上报告说,他们发现人体内一种基因拥有遏制癌细胞转移的功能,这将有助于弄清癌细胞转移的机制并开发出新药。 该校研究生院教授今川正良率领的研究小组注意到,一种名为“fad104”的基因与细胞移动等有关,因此通过实验调查了其是否与癌细胞的转移有关。该基因能促进脂肪细胞分化,在肺的形成过程中,还对II型肺泡
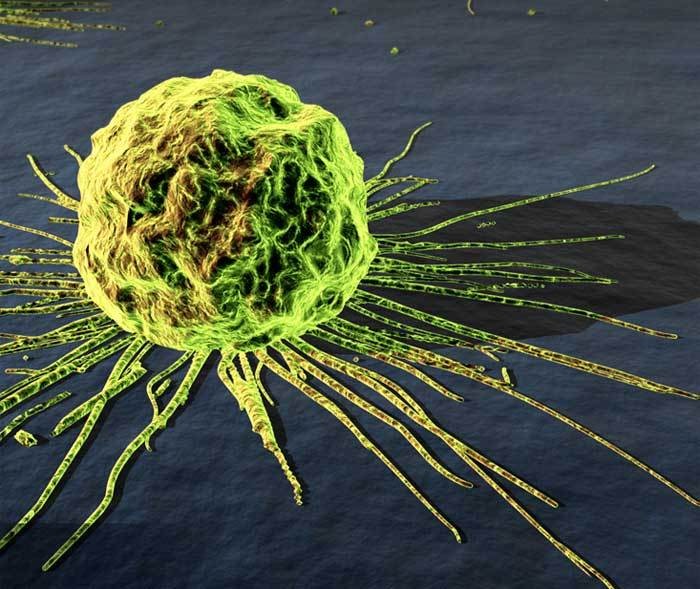
日本名古屋市立大学的一个研究小组在新一期的美国在线科学杂志《公共科学图书馆综合卷》上报告说,他们发现人体内一种基因拥有遏制癌细胞转移的功能,这将有助于弄清癌细胞转移的机制并开发出新药。
该校研究生院教授今川正良率领的研究小组注意到,一种名为“fad104”的基因与细胞移动等有关,因此通过实验调查了其是否与癌细胞的转移有关。该基因能促进脂肪细胞分化,在肺的形成过程中,还对II型肺泡上皮细胞的分化和成熟以及骨骼的形成等发挥重要作用。
研究小组发现,癌细胞会借助血管等在体内移动。研究人员对人类恶性黑色素瘤的癌细胞进行处理,减弱了其中“fad104”基因的功能后发现,癌细胞更容易进入实验鼠的血管。相反,如果强化癌细胞中“fad104”基因的功能,并将这种癌细胞注射到实验鼠尾部,癌细胞向肺部的转移则急剧减少。
研究小组指出,这一发现促进了对癌细胞转移分子机制的认识,并有助于推动开发新的治疗药物。
原始出处:
Katoh D1, Nishizuka M1, Osada S1, Imagawa M1.Fad104, a Positive Regulator of Adipocyte Differentiation, Suppresses Invasion and Metastasis of Melanoma Cells by Inhibition of STAT3 Activity.PLoS One. 2015 Feb 11;10(2):e0117197. doi: 10.1371/journal.pone.0117197. eCollection 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Plos one#
49
很不错学习了
145
很不错学习了
148
很不错
140
?学习了
134
#癌细胞#
40
#细胞转移#
54
#癌细胞转移#
67
Good
131