AP&T: 经会阴超声检查肠壁厚度的改善可预测活动性溃疡性结肠炎的治疗的效果
2022-05-04 xuyihan MedSci原创
B型超声检查(type-B ultrasonic ),俗称“B超”,是患者在就诊时经常接触到的医疗检查项目。在临床上,它被广泛应用于心内科、消化内科、泌尿科和妇产科疾病的诊断。
溃疡性结肠炎 (UC) 是一种炎症性肠病,反复发作,导致结肠慢性炎症。炎症通常在直肠中最严重并延伸到近端结肠。中度至重度活动性疾病可以通过诱导治疗进行治疗,例如皮质类固醇、生物制剂或小分子药物。在现实世界的实践中,只有大约一半的患者可以达到临床缓解。因此,早期确定对诱导治疗的反应是活动性 UC 治疗非常重要的指标。内窥镜检查在评估 UC 疾病状态中起着关键作用。然而,由于其侵入性,它不适合在短时间内频繁监测。测量粪便钙卫蛋白 (FC) 的侵入性较小;然而,由于它在活动性疾病期间变化很大,因此它作为对诱导治疗的反应的预测指标并不是很有用。相比之下,肠道超声检查因其微创特性而易于重复,并且可以评估静止和活动性疾病中 UC 的内镜严重程度。然而,经腹超声 (TAUS) 可能无法很好地显示直肠;因此,在之前的报告中,研究人员指出了经会阴超声 (TPUS) 在预测直肠疾病活动方面的有用性,患者接受度很高。超声参数,如肠壁厚度 (BWT) 和肠壁流量 (BWF),可能会在诱导治疗后 12 周内与症状改善相关。在这项研究中,研究人员旨在调查肠道超声检查,尤其是 TPUS,是否可用于预测早期诱导治疗的临床反应。

这项单中心前瞻性研究中,研究人员对接受诱导治疗的活动性 UC 患者进行了相关分析,在第 8 周时对患者的临床缓解的超声预测指标进行了测量,并与粪便钙卫蛋白和 C 反应蛋白进行比较(在基线、第 1 周和第 8 周测量)。使用多变量回归模型和接受者操作特征曲线分析评估预测因素。

本项研究共分析了 100 名患者,其中 54 名在第 8 周达到临床缓解。基线生物标志物和超声参数值不能预测临床缓解。相比之下,使用经会阴超声测量的直肠肠壁厚度从基线到第 1 周的变化是第 8 周缓解的独立预测因子(调整后的比值比与减少 1 毫米相关:1.90 [95% 置信区间,1.22-2.95] )。在对 1 周内未达到缓解的患者进行的亚组分析中,直肠肠壁厚度变化的预测值仍然很高(AUC = 0.77 [95%CI,0.61-0.88])。
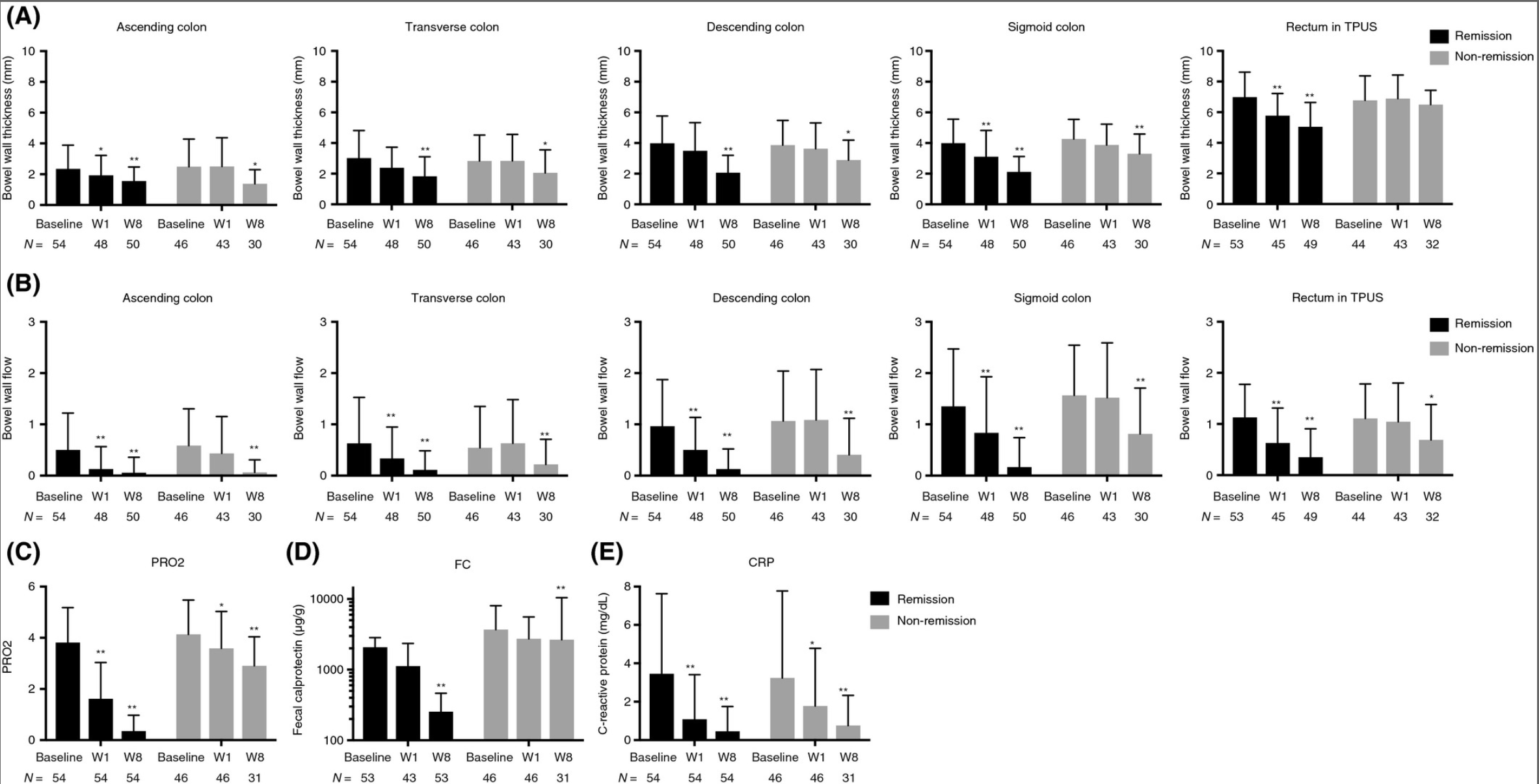
图:超声不同测量值对于疾病改善情况的预测
本项研究证实在第 1 周使用经会阴超声测量直肠肠壁厚度的UC患者如果出现改善则可预测其治疗成功,并可能有助于 UC 早期诱导治疗过程中的决策。
原始出处:
Shintaro Sagami. Et al. Early improvement in bowel wall thickness on transperineal ultrasonography predicts treatment success in active ulcerative colitis. Aliment Pharmacol Ther.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#活动性溃疡性结肠炎#
103
#溃疡性#
146
#活动性#
90
#超声检查#
83
#会阴#
135