构建导航护士在ERAS 腹腔镜肝切除术中的管理路径:护患沟通我有一套
2019-05-16 杨艳英 健康界
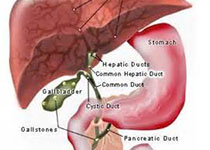
构建导航护士在ERAS腹腔镜肝叶切除术中的管理路径一、项目背景近年,加速康复外科(Enhanced Recovery After Surgery )的安全性和有效性被越来越多的研究证实,目前该理念被运用于多个学科。外科医生、护理、麻醉、营养、康复科、心理等多学科组成的ERAS-MDT团队是加速康复外科运行的组要模式,得到国内专家的普遍认同。尽管如此,在工作开展过程中仍暴露出诸多问题,其中最为突
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肝切除#
76
#ERA#
44
#切除术#
58
#管理路径#
74
#腹腔镜肝切除术#
85
#腹腔镜#
70
#肝切除术#
85