Cancer Treat Rev:如何实现结直肠癌分子亚型与临床病理表型的互通转化?
2017-06-03 月下荷花 肿瘤资讯
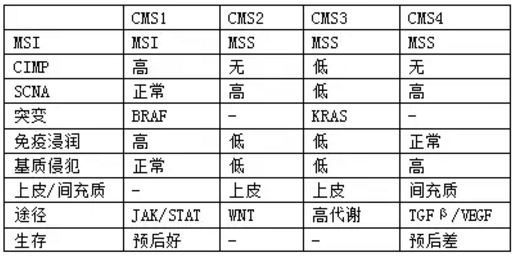
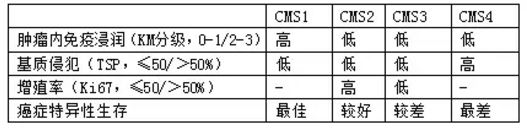
2015年提出CRC的共识分子亚型:CMS1-MSI免疫型,CMS2-经典型,CMS3-代谢型,和CMS4-间充质型,并对上述亚型进一步分析了CpG甲基化(CIMP)、体拷贝数分析(SCNA)、突变、KRAS和BRAF突变、癌基因信号瀑布和基质侵犯、免疫浸润等特征(表1)。CMS4的无复发生存最差,5年生存60%,而CMS1为75%,CMS2/3为73%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床病理#
74
#TREAT#
83
学习了,谢谢分享
100
#表型#
53
#结直肠#
72
#分子亚型#
62
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了,点个赞吧!
87
学习了谢谢分享。
75
学习了谢谢分享。
92
林奇综合症的预后更差
1