Front Oncol:EBV感染相关胃癌(EBVaGC)的临床病理特征和化疗应答
2021-09-25 yd2015 MedSci原创
研究表明,EBV相关胃癌(EBVaGC)具有独特的临床病理学特征并且对化疗的应答较差。同时,新辅助化疗并不适合该类患者。
基于TCGA数据库的多组测序的结果,目前将胃癌分为四个亚型:微卫星不稳定(MSI)、EBV病毒(EBV)阳性、基因组稳定(GS)和染色体不稳定(CIN)。EBV相关胃癌(EBVaGC)约占胃癌的9%,表现出大量淋巴细胞浸润、全基因组高甲基化、和程序性死亡配体1 (PD-L1)高表达等特点。根据组织病理学特征免疫治疗被用于治疗EBVaGC。但是PD-1/PD-L1单药治疗的客观有效率(ORR)仅为0~20%。因此,EBVaGC的最佳治疗方案尚不清楚。近期,来自我国北京大学肿瘤医院的团队开展了回顾性研究,评估EBV相关胃癌(EBVaGC)的临床病理学特征和化疗应答。相关结果发表在Frontiers in Oncology杂志上。
研究回顾性纳入2013年3月至2020年7月在北京肿瘤医院诊断为EBVaGC的患者并记录其临床病理特征。然后计算无病生存(DFS),并用Cox比例回归模型检验影响DFS的变量。
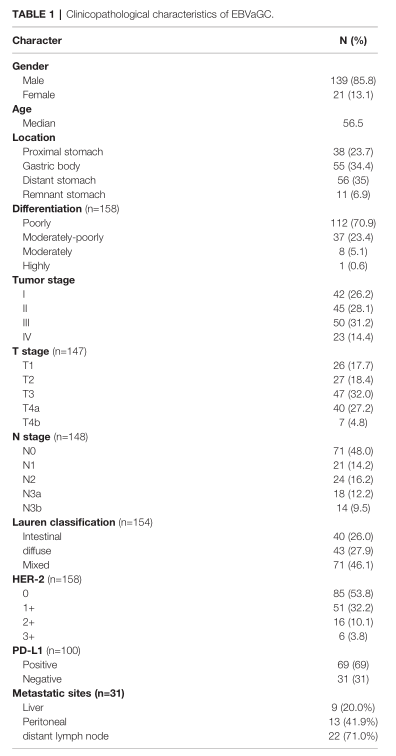
最终纳入160例EBVaGC患者进行分析。其中85.8%(139/160)为男性。平均年龄为56.5岁。35%(56/160)的患者有饮酒史,55%(88/160)的患者吸烟。I期42例(26.2%),II期45例(28.1%),III期50例(31.2%),IV期23例(14.4%)。位于胃近端38例(23.7%),胃体55例(34.4%),胃远端56例(35%),残胃11例(6.9%)。96.9%(155/160)为腺癌。
100例患者有明确的PD-L1结果,其中69%的患者阳性,中位CPS为10。PD-L1阳性组与PD-L1阴性组在肿瘤分期(χ2= 0.215, p = 0.898)、T分期(χ2 = 0.850, p = 0.860)和N分期(χ2= 0.215, p = 0.741)方面差异无统计学意义。158例确诊患者中只有6例(3.8%)出现HER-2 (3+), HER-2(0)、HER-2(1+)、HER-2(2+)患者分别为85例(53.8%)、51例(32.3%)、16例(10.1%)。所有患者均为pMMR和MSS。
临床特征
33例患者术前接受新辅助治疗,所有患者均行R0切除术。确定为肿瘤退缩级别(TRG1)、TRG2和TRG3的患者分别为5例(15.2%)、16例(48.5%)和12例(36.4%)。
31例患者接受了一线化疗。其中肝转移9例,腹膜转移13例,远处淋巴结转移22例。ORR为33.3%,DCR为61.9%。根据PD-L1 (p = 0.58)或Ki-67 (p = 0.58)状态评估肿瘤应答间没有差异。
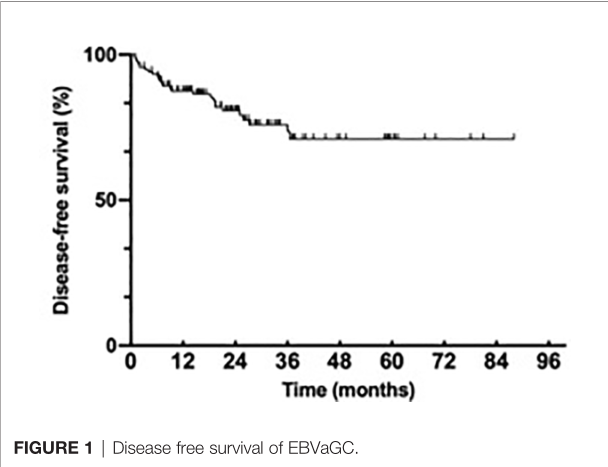
147例患者接受手术治疗,27例复发; 3年DFS率为71.0%。中位DFS尚未达到。
DFS
新辅助化疗组(p = 0.010)、肿瘤晚期(p = 0.003)、T期(p = 0.002)、N期(p = 0.002)、PD-L1阴性(p = 0.048)、血管侵犯(p = 0.013)的患者DFS较差。
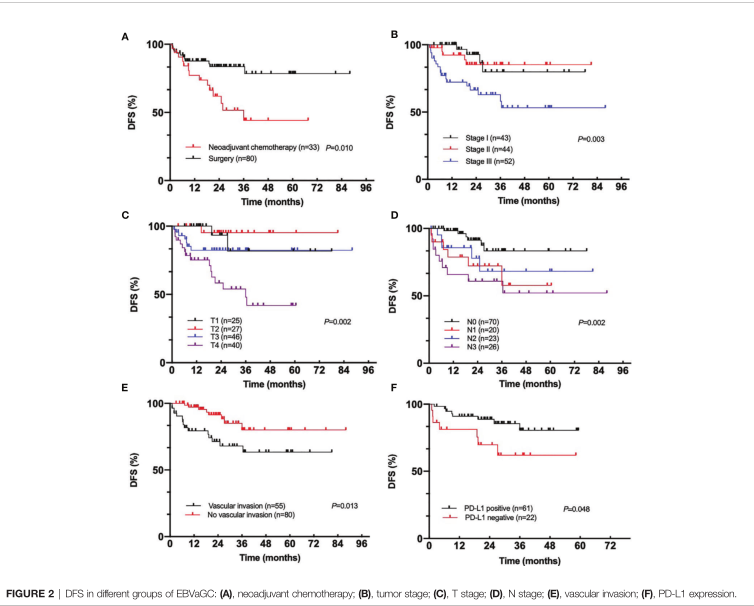
不同亚组DFS比较
在多变量Cox回归模型中,血管侵犯(p = 0.013)是DFS的独立危险因素。

DFS危险因素
综上,研究表明,EBV相关胃癌(EBVaGC)具有独特的临床病理学特征并且对化疗的应答较差。同时,新辅助化疗并不适合该类患者。
原始出处:
Xie T, Peng Z, Liu Y, et al. (2021) Clinicopathological Characteristics and Response to Chemotherapy in Treatment-Naïve Epstein–Barr Virus Associated Gastric Cancer: A Retrospective Study. Front. Oncol. 11:611676. doi: 10.3389/fonc.2021.611676
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#临床病理#
93
#Oncol#
58
#病理特征#
88
#EBV#
80
感谢分享,收藏了
81
学习学习
77