Cell Res:分泌蛋白CST6调节乳腺癌骨转移
2012-06-18 bo 生物谷
6月12日,Cell Research杂志报道了调节乳腺癌骨转移的分泌蛋白的最新研究进展。骨转移是乳腺癌的常见并发症,也是其致死、致残的重要原因。在转移过程中,分泌蛋白在癌细胞与宿主基质的相互作用上发挥重要的作用。 为了鉴定与乳腺癌转移相关的分泌蛋白,研究者利用无标记蛋白组分析比较了四种具有不同骨转移能力的来源于人乳腺癌细胞MDA-MB-231(MDA231) 的细胞系的蛋白分泌组。在培养过有骨
6月12日,Cell Research杂志报道了调节乳腺癌骨转移的分泌蛋白的最新研究进展。骨转移是乳腺癌的常见并发症,也是其致死、致残的重要原因。在转移过程中,分泌蛋白在癌细胞与宿主基质的相互作用上发挥重要的作用。
为了鉴定与乳腺癌转移相关的分泌蛋白,研究者利用无标记蛋白组分析比较了四种具有不同骨转移能力的来源于人乳腺癌细胞MDA-MB-231(MDA231) 的细胞系的蛋白分泌组。在培养过有骨转移能力的癌细胞的培养基中,共发现128种蛋白的水平一致性上调或下调。这些发生水平改变的蛋白的功能包括受体结合和肽酶抑制。
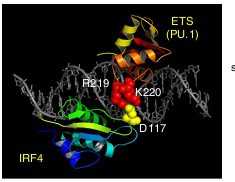
通过对乳腺癌转录组的分析,研究者选取在骨转移癌细胞中下调的半胱氨酸蛋白酶抑制剂E/M(CST6)作为进一步研究的对象。其研究结果显示,CST6抑制乳腺癌的细胞增殖,集落形成,迁徙和侵袭。肿瘤来源的可溶性CST6介导针对癌细胞运动能力的功能抑制。更重要的是,在癌细胞中表达CST6可显著缓解实验小鼠的溶骨性转移和死亡。而CST6下调明显增强癌细胞的骨转移和缩短小鼠寿命。
总之,该研究提供了骨趋向性乳腺癌系统的分泌蛋白质组分析。它还证实,分泌性CST6的确是乳腺癌骨转移的抑制因子。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Differential secretome analysis reveals CST6 as a suppressor of breast cancer bone metastasis
Lei Jin1,*, Yan Zhang2,*, Hui Li1, Ling Yao2, Da Fu1, Xuebiao Yao3, Lisa X Xu2, Xiaofang Hu2 and Guohong Hu1
Bone metastasis is a frequent complication of breast cancer and a common cause of morbidity and mortality from the disease. During metastasis secreted proteins play crucial roles in the interactions between cancer cells and host stroma. To characterize the secreted proteins that are associated with breast cancer bone metastasis, we preformed a label-free proteomic analysis to compare the secretomes of four MDA-MB-231 (MDA231) derivative cell lines with varied capacities of bone metastasis. A total of 128 proteins were found to be consistently up-/down-regulated in the conditioned medium of bone-tropic cancer cells. The enriched molecular functions of the altered proteins included receptor binding and peptidase inhibition. Through additional transcriptomic analyses of breast cancer cells, we selected cystatin E/M (CST6), a cysteine protease inhibitor down-regulated in bone-metastatic cells, for further functional studies. Our results showed that CST6 suppressed the proliferation, colony formation, migration and invasion of breast cancer cells. The suppressive function against cancer cell motility was carried out by cancer cell-derived soluble CST6. More importantly, ectopic expression of CST6 in cancer cells rescued mice from overt osteolytic metastasis and deaths in the animal study, while CST6 knockdown markedly enhanced cancer cell bone metastasis and shortened animal survival. Overall, our study provided a systemic secretome analysis of breast cancer bone tropism and established secreted CST6 as a bona fide suppressor of breast cancer osteolytic metastasis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#蛋白C#
53
#分泌蛋白#
47
#CEL#
52
#CST6#
68
#分泌#
0
#ST6#
61
#Cell#
52