European Radiology:Gd-EOB-DTPA增强MRI,实现HCC微血管浸润的无创评估!
2022-03-09 shaosai MedSci原创
微血管侵犯(MVI)是肝细胞癌(HCC)复发和影响预后的一个重要风险因素。对于有MVI的HCC患者,应扩大手术切除和射频消融的边缘范围,同时也应考虑将肝移植纳入替代治疗方法之一。
 微血管侵犯(MVI)是肝细胞癌(HCC)复发和影响预后的一个重要风险因素。对于有MVI的HCC患者,应扩大手术切除和射频消融的边缘范围,同时也应考虑将肝移植纳入替代治疗方法之一。因此,术前对MVI的准确预测有助于临床医生做出更合理的术式决定。然而,MVI的诊断主要依赖于有创的活检或术后病理,因此很难常规获得。
微血管侵犯(MVI)是肝细胞癌(HCC)复发和影响预后的一个重要风险因素。对于有MVI的HCC患者,应扩大手术切除和射频消融的边缘范围,同时也应考虑将肝移植纳入替代治疗方法之一。因此,术前对MVI的准确预测有助于临床医生做出更合理的术式决定。然而,MVI的诊断主要依赖于有创的活检或术后病理,因此很难常规获得。
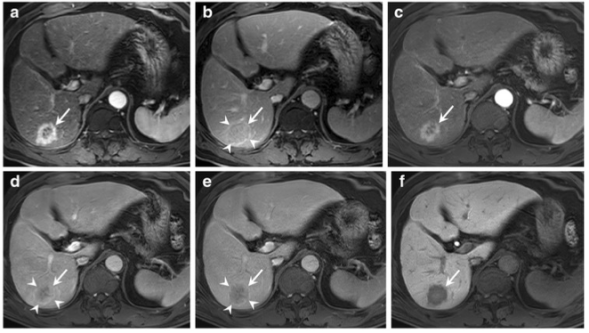
目前,医学影像学已被用于HCC术前的MVI预测,包括肿瘤大小、形态学特征、增强表现,同时也可用于分析肿瘤微环境的变化。然而,以往预测MVI的数据仍有争议。Gd-EOB-DTPA作为一种肝细胞特异性造影剂,为HCC的诊断提供了额外的诊断信息。Gd-EOB-DTPA MRI可用于定量和定性评估HCC发展过程中的瘤内和瘤周影像学特征。
此外,血小板与淋巴细胞比率(PLR)和碱性磷酸酶(ALP)等生化指标指标也都与MVI密切相关。[ALP(U/L)+γ-谷氨酰转肽酶(GGT)(U/L)]/淋巴细胞数(×109/L)比值(AGLR)是评价HCC进展和预后的一种新型生化指标。越来越多的证据表明,ALP是一种与癌症相关的血清酶,其升高可能在肿瘤增殖中起重要作用。GGT是一种无处不在的上皮酶,GGT的升高会诱发肝功能受损和代谢异常。淋巴细胞可能参与免疫调节并诱导细胞凋亡。然而,据我们所知,临床上对AGLR和MVI之间的确切相关性仍不明确。
近日,发表在European Radiology杂志的一项研究利用Gd-EOB-DTPA MRI结合生化指标建立了一个实用的、简单明了的用于HCC术前预测MVI的评分模型,并通过独立的外部验证对其诊断价值进行了评价。
本项回顾性研究纳入了我院2014年至2020年的129例HCC患者。根据Gd-EOB-DTPA MRI上的瘤内和瘤周特征以及生化指标,建立了一个用于术前预测MVI的评分模型,并根据术后病理结果检验了诊断效果。该评分模型在63名HCC患者的独立队列中得到进一步的外部验证。
本研究进行了逻辑回归分析,确定了与MVI相关的五个参数,包括最大肿瘤直径、肝胆期瘤周低信号、包膜不完整、表观扩散系数(ADC)和[碱性磷酸酶(ALP)(U/L)+γ-谷氨酰转肽酶(GGT)(U/L)] / 淋巴细胞计数(×109/L)比率(AGLR)。基于这五个参数建立了一个评分模型,其预测MVI的准确性、敏感性、特异性、PPV和NPV分别为93.6%、94.7%、93.2%、85.7%和97.6%,评分>8为阈值。
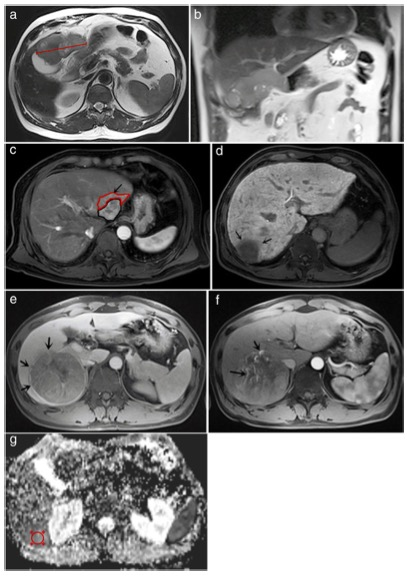
图 MR特征表现的示例图。(a)和(b)同一患者在轴位和冠位图像上有不规则的分叶状病变。最大直径取自病变最大层面上的两个最远点的连接线长度(a)。其他表现为动脉期的瘤周强化(红色轮廓代表瘤周强化,黑色轮廓代表肿瘤)(c)、肝胆期的瘤周低强度(d)、包膜不完整(e)和瘤内动脉样强化(f)。肿瘤的ADC值由三次测量的平均值获得,并划定了ROI以避免异质成分如坏死或出血(g)的干扰。
本研究为术前预测HCC的MVI情况开发了一个可靠的评分模型,该模型具有较高的准确性、敏感性和特异性,可协助临床医生根据HCC的强化MRI征象和生物学特征实施更合理的干预措施及更精确和个性化的治疗。
原文出处:
Kun Zhang,Shuang-Shuang Xie,Wen-Cui Li,et al.Prediction of microvascular invasion in HCC by a scoring model combining Gd-EOB-DTPA MRI and biochemical indicators.DOI:10.1007/s00330-021-08502-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
48
#tPA#
59
#HCC#
55
#微血管#
51