Nat Med:Danuglipron(PF-06882961)治疗2型糖尿病的疗效分析
2021-06-15 xiaozeng MedSci原创
据估计,全球有超过4.6亿人患有糖尿病,预计到2030年糖尿病患者人数将超过5.7亿。在这些人群中,大约90%的患者患有2型糖尿病(T2D)。尽管T2D具有可用的治疗策略,但在美国只有约50%的患者达
据估计,全球有超过4.6亿人患有糖尿病,预计到2030年糖尿病患者人数将超过5.7亿。在这些人群中,大约90%的患者患有2型糖尿病(T2D)。尽管T2D具有可用的治疗策略,但在美国只有约50%的患者达到低于治疗目标的HbA1c(糖化血红蛋白)水平。
GLP-1R(胰高血糖素样肽1受体)的激活能够刺激胰岛素的释放,病以葡萄糖依赖性方式抑制胰高血糖素的分泌,最终导致血糖的降低和体重的减轻,其是治疗T2D和肥胖症的一种治疗策略。因此,寻找治疗性GLP-1R激动剂对于T2D的治疗尤为重要。
在该研究中,研究人员开发了一种口服小分子GLP-1R激动剂danuglipron (PF-06882961),并在人源化小鼠模型中发现其与注射肽GLP-1R激动剂具有相当的功效。
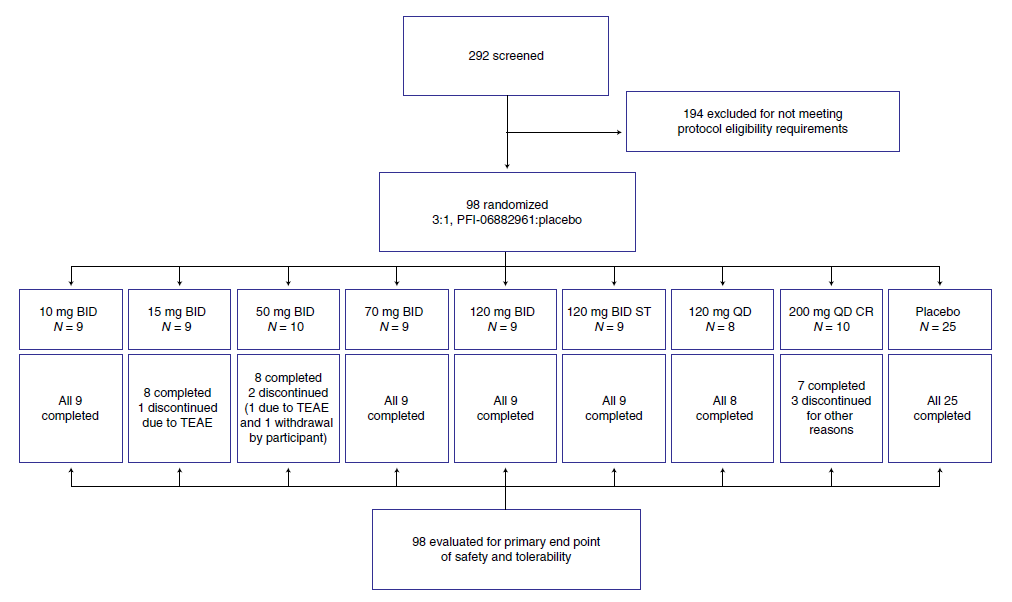
因此,研究人员开展并完成了一项安慰剂对照、随机、双盲、多次递增剂量的1期临床研究(NCT03538743),在该研究中,研究人员招募了98名服用二甲双胍背景的T2D患者,将他们随机分配并接受多次递增剂量的danuglipron或安慰剂治疗28天、这些病例跨越了八个队列。
参与者数据
研究的主要结果为不良事件(AE)、安全测试、患者生命体征和十二导联心电图的评估。大多数的AE是轻微的,最常见的是恶心、消化不良和呕吐等。
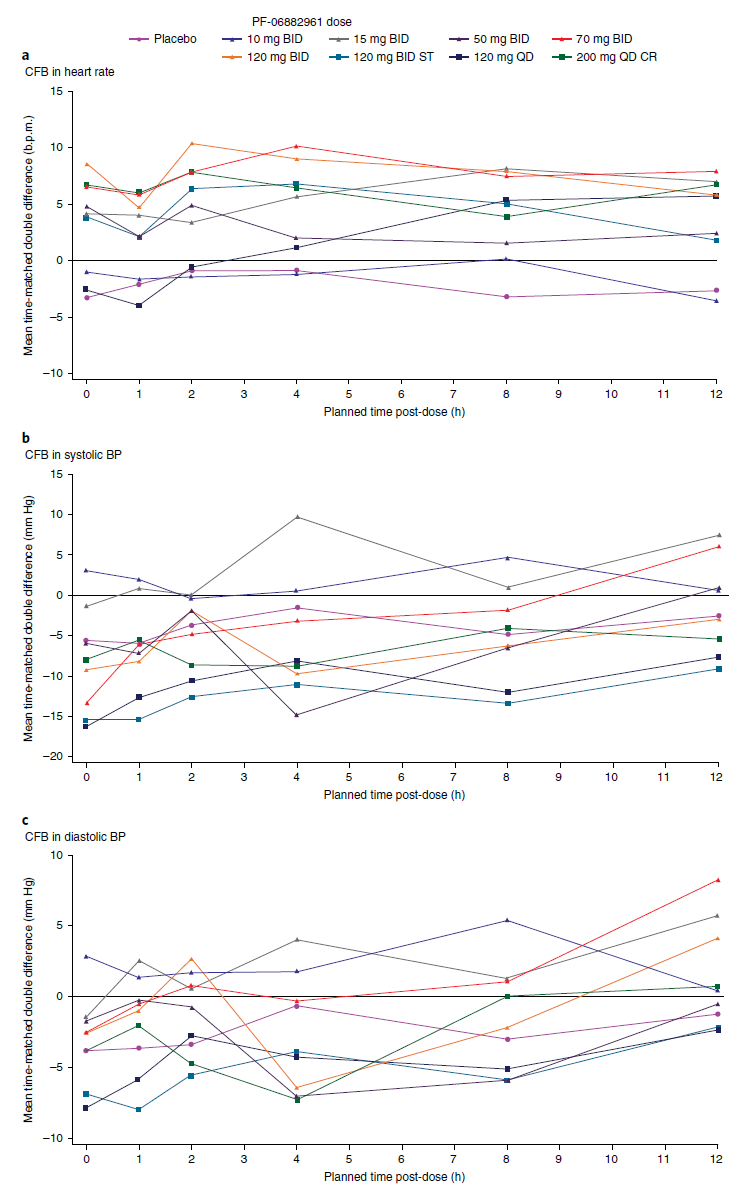
结果显示,各组间并无具有临床意义的AE发生。在第28天使用danuglipron治疗时,心率通常会增加,但并无报告相关心率AE的发生。相比于安慰剂,第28天使用danuglipron治疗时收缩压略有下降,舒张压变化相似。患者的心电图结果并无临床上的差异。
第28天的生命体征相比基线的变化
总而言之,该项T2D研究揭示,患者对danuglipron的耐受性良好,其安全性与GLP-1R激动剂的作用机制一致。
原始出处:
Saxena, A.R., Gorman, D.N., Esquejo, R.M. et al. Danuglipron (PF-06882961) in type 2 diabetes: a randomized, placebo-controlled, multiple ascending-dose phase 1 trial. Nat Med (14 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
62
#疗效分析#
73
#PRO#
90
#Med#
60
谢谢梅斯提供这么好的信息,学到很多
79
谢谢MedSci提供最新的资讯
71