NEJM:山地车越野时颈部被树枝穿刺伤的案例报道
2015-07-26 MedSci MedSci原创
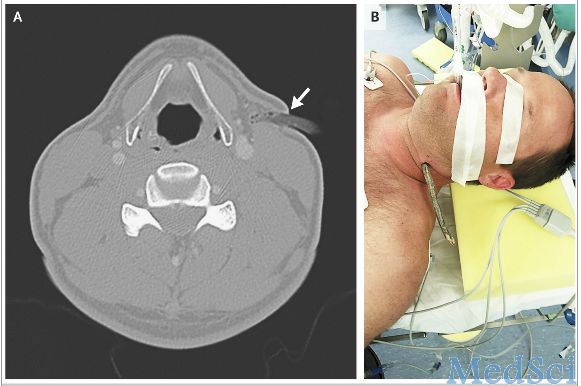
近日,一名40岁的健康男子骑山地车越野的时,中途意外摔倒,被一根树枝从颈部侧方穿刺伤。事后,该男子没有试图当场拔出树枝,而是自行到医院急诊科就诊。CT血管造影显示树枝在颈部左侧甲状腺软骨水平的软组织内,一直延伸到颈阔肌和胸锁乳突肌的前缘(如图A箭头所指处)。该树枝从皮肤表面延伸至皮下约1.6cm深,所幸的是没有出现血管和气道损伤的迹象(如图A)。一般的情况下,颈部的穿刺伤会损伤到血管、呼吸道、颈椎

一般的情况下,颈部的穿刺伤会损伤到血管、呼吸道、颈椎和颈部神经等。当血管结构受到损伤出现大出血时,通常会选择穿刺的异物在放射科检查和手术前都不拔出,这样有利于对出血的部位有止血的作用。
该男子在手术中,主刀医生对其颈部异物取出后,对伤口进行探查、消毒和关闭伤口(如图B所示)。
术后,该男子的生命体征平稳,恢复得很好。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错,赞一个
133
这篇文章有一定深度
140
是一篇不错的文章
163
值得进一步关注
138
这。。。
113
#穿刺#
81
#颈部#
58
这也能发表在NEJM?
111
好吧
93
有意义的事
113