



实体瘤疗效评价标准(RECIST1.1)是以瘤体大小变化来评估疗效,这也是当前肿瘤治疗疗效评判的金标准。缺陷:
①以单一影像学资料反映局部的疗效来判定疾病的整体治疗效果;
②瘤体缩小持续4周仅仅反映近期疗效;
③以单一的客观标准来反映复杂的病变,忽视了肿瘤负荷的变化,而这往往最能反映出患者的生活质量及生存时间。
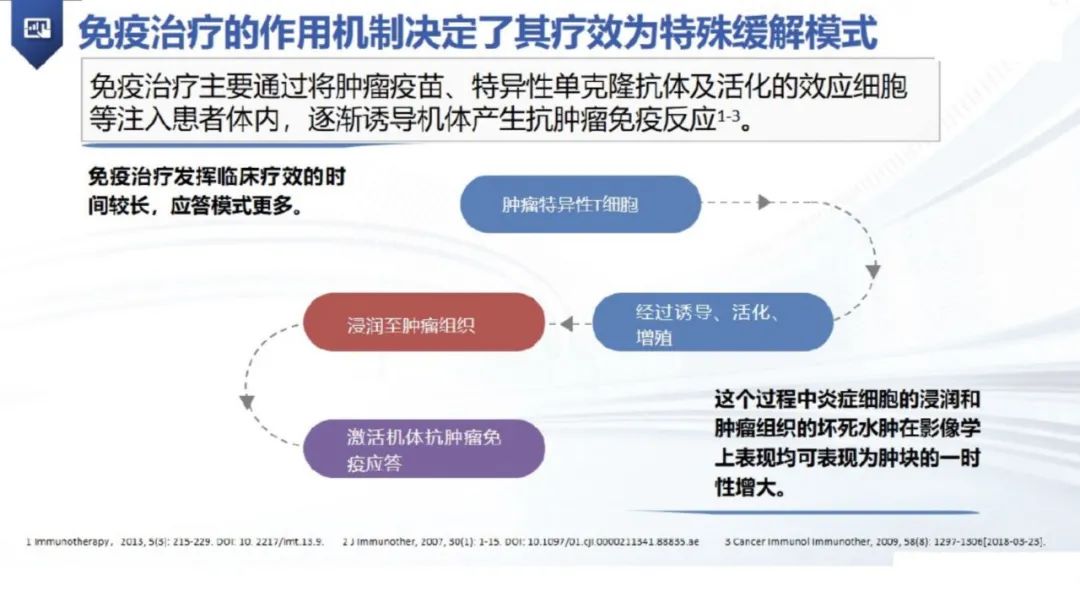
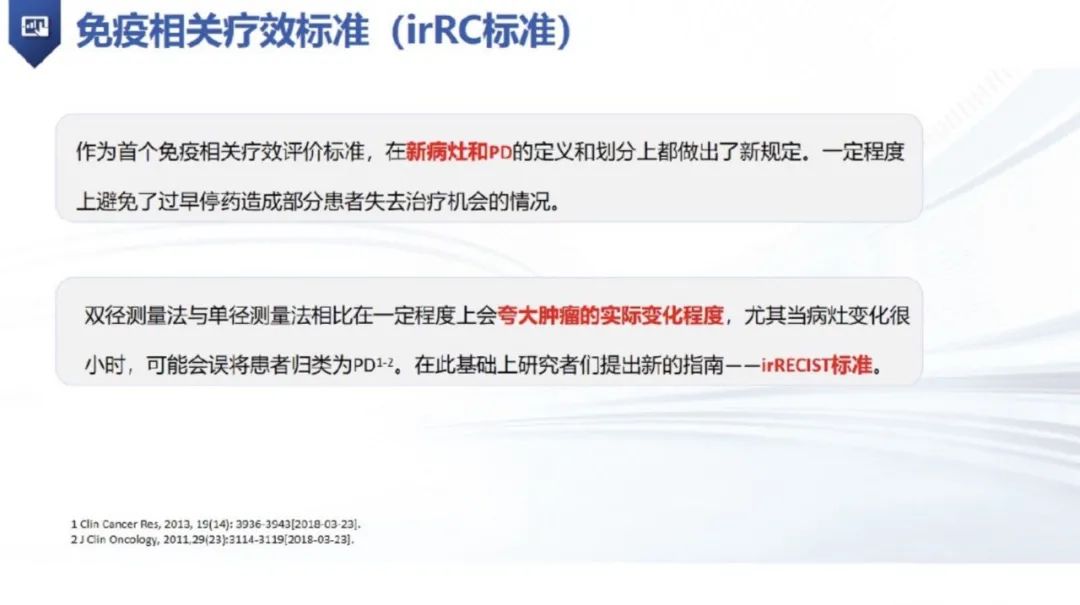
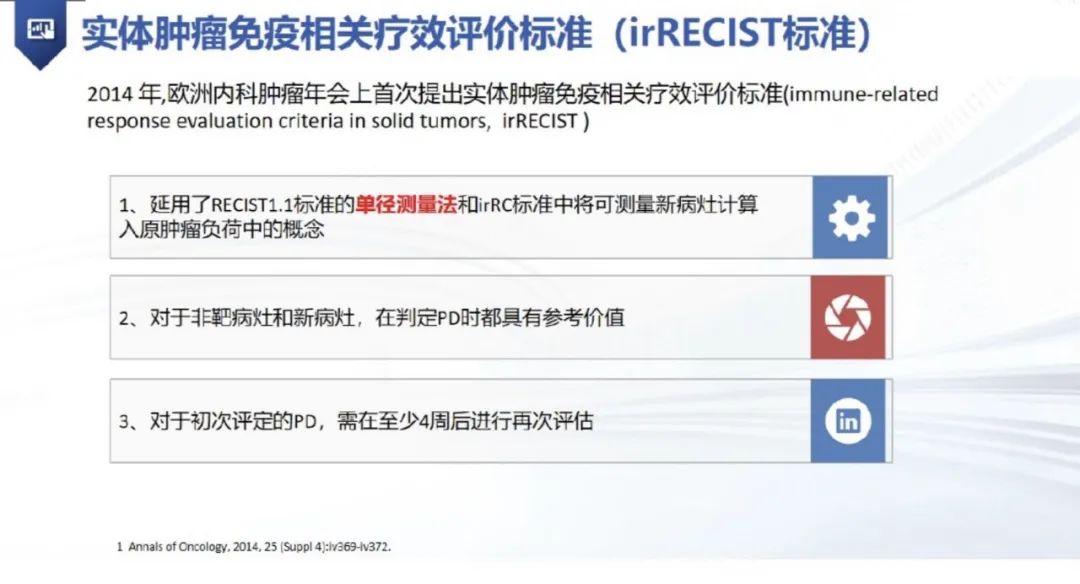
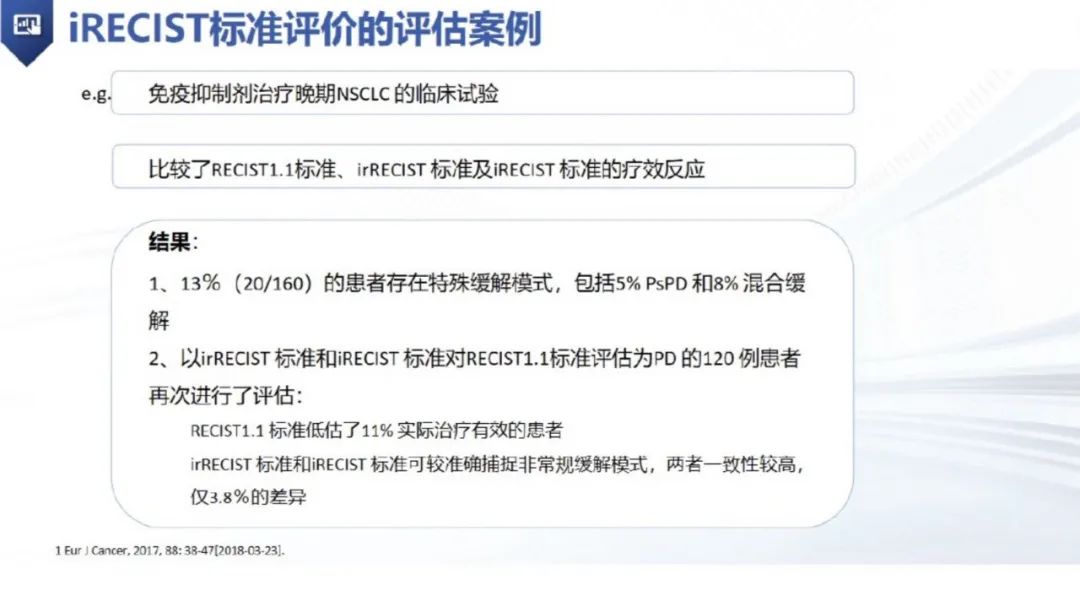
按照传统的疗效评价体系来评价肿瘤免疫治疗的疗效,往往会由于没有明显的瘤体改变而得出治疗无效的结论,并且传统的疗效评价体系不足以捕获假性进展,可能会低估免疫检查点阻断的治疗益处。






“临床状态稳定”定义:无功能状态(per-formance status,PS)评分增加;无疾病相关的临床症状加重,如疼痛、呼吸困难、食欲、体重下降和患者自身的感觉等;没有增加疾病相关症状的治疗措施,如镇痛、放疗或其他姑息治疗。



备注:本文来源网络,内容有增减。小编已对内容进行审核。
参考文献
[1]蒋琼慧,路泽军,杨平.肿瘤免疫治疗疗效评价标准——iRECIST解读[J].转化医学杂志,2020,9(1):57-60.
[2]Seymour L, Bogaerts J, Perrone A, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017 Mar;18(3):e143-e152. doi: 10.1016/S1470-2045(17)30074-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#疗效评价#
0
#RECIST#
88
#期刊论坛#
79
#CIS#
92
#实体肿瘤#
95
#评价#
81
#评价标准#
68
很好
71