Prostate Cancer P D:两种消融技术治疗放射复发前列腺癌的长期结果
2020-09-06 AlexYang MedSci原创
前列腺癌放疗后复发的男性,进一步治疗仍旧是一个挑战。常规的雄激素剥夺疗法(ADT)挽救方案有不良影响。另外,只有选择的部分男性可以进行挽救性治疗。最近,有研究人员阐释了两种全腺消融技术-冷冻疗法(sC
前列腺癌放疗后复发的男性,进一步治疗仍旧是一个挑战。常规的雄激素剥夺疗法(ADT)挽救方案有不良影响。另外,只有选择的部分男性可以进行挽救性治疗。最近,有研究人员阐释了两种全腺消融技术-冷冻疗法(sCT)和高强度聚焦超声(sHIFU)的长期肿瘤学结果。

研究中共有187名男性进行了sCT,113名男性进行了sHIFU。整个队列的平均(SD)年龄为69.9(5.9岁),放射前PSA中值为9.6 ng/ml(IQR 6.1-15.2),挽救前PSA中值为 4.5 ng/ml(IQR 2.8-7.0)。总的随访时间中值为116个月(IQR 67.5-173.8)。共有170名(57.6%)发展为生化复发(BCR),68名(23.4%)发生转移,143名(49.3%)开始进行ADT治疗,58名(20.1%)发展为CRPC,162名(56%)患者死亡,其中59名(36.4%)为因前列腺癌死亡。多变量分析中,sHIFU(HR 1.65,95%CI 1.15-2.36,p=0.006)和救治前PSA(HR 1.09,95%CI 1.06-1.13,p<0.0001)与较高的BCR风险相关。相似地,sHIFU患者有更高的CRPC风险(HR 2.31,95%CI 1.23-4.35,p=0.009)。PCSM的10年累积发生率(两种治疗)为16.5%(95%CI 12.2-21.4%),20年时为28.4%(95%CI 22.1-34.9%),治疗方式之间没有差异。挽救前PSA是测量的肿瘤学结果的常用预测因子。
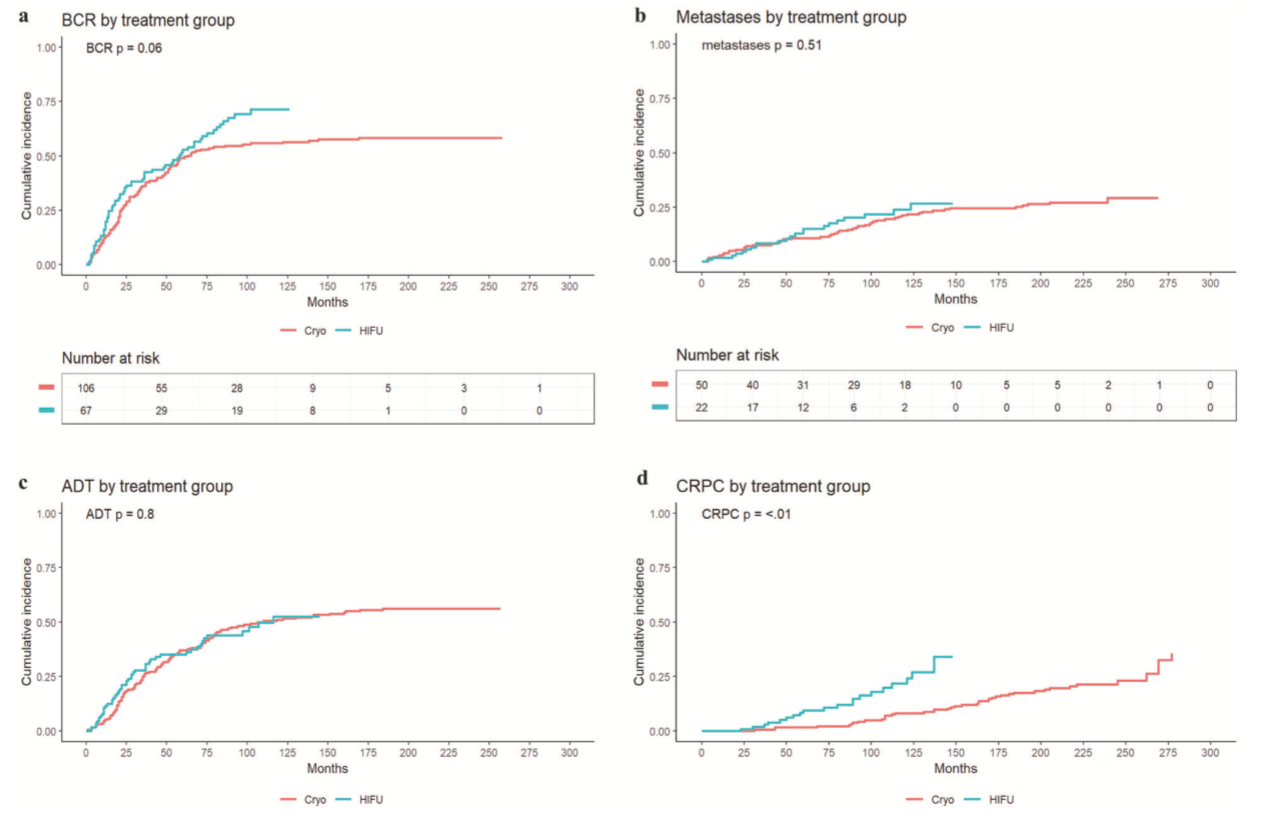

两种消融技术的肿瘤参数累积发生率
最后,研究人员指出,尽管sHIFU的BCR和CRPC率较高,但与sCT相比,PCSM没有差异。两种消融技术的长期肿瘤学数据表明,10年随访后只有50%的患者开始ADT治疗。
原始出处:
Shiva M. Nair, Max Peters, Piet Kurver et al. Long-term outcomes of two ablation techniques for treatment of radio-recurrent prostate cancer. Prostate Cancer P D. August 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#长期结果#
90
#Prostate Ca#
75
前列腺消融是要用超声引导吗
128
#消融技术#
114
#ROS#
87
#消融#
91
#PRO#
83
学习
132
前列腺癌相关研究,学习了,谢谢梅斯
91