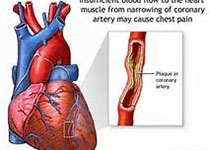
JAHA:胸段硬膜外麻醉可作为难治性室速的治疗选择
2017-11-22 MedSci MedSci原创
目前,一些调节自主神经系统的新疗法,比如胸段硬膜外麻醉(TEA),在一些小型的系列研究中被证实对难治性室速(VT)有较好的疗效。然而,这是否可以真正作为治疗难治性室速的一个方法尚未阐明。本研究回顾分析了2005年至2016年11例接受胸段硬膜外麻醉的难治性室速患者,对其临床特征、预后结局和治疗管理进行了全面分析。在临床表现上,有7例(64%)患者为持续性室速,3例(27%)患者为多相室速,8例(7
目前,一些调节自主神经系统的新疗法,比如胸段硬膜外麻醉(TEA),在一些小型的系列研究中被证实对难治性室速(VT)有较好的疗效。然而,这是否可以真正作为治疗难治性室速的一个方法尚未阐明。本研究回顾分析了2005年至2016年11例接受胸段硬膜外麻醉的难治性室速患者,对其临床特征、预后结局和治疗管理进行了全面分析。在临床表现上,有7例(64%)患者为持续性室速,3例(27%)患者为多相室速,8例(73%)患者为单相室速,其他潜在的临床表现包括5例(45%)非缺血性心肌病,3例(27%)缺血性心肌病,肥厚型心肌病、Brugada综合征和心脏脂肪瘤各1例(9%)。共有5例(45%)患者对TEA有明显反应,1例(9%)患者对TEA有部分反应,在5例有明显反应的患者中,4例为持续性室速。本研究结果显示,有超过一半的难治性室速患者对胸段硬膜外麻醉是有反应的,TEA可作为难治性室速尤其是持续性室速患者治疗的选择。原始出处:Duc H et al.Thoracic Epidural Anesthesia Can Be Effective for the Short‐Term Management of
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬膜外#
61
#治疗选择#
40
#硬膜外麻醉#
69
#AHA#
59
#室速#
54
#难治性#
0
学习了.谢谢.
72