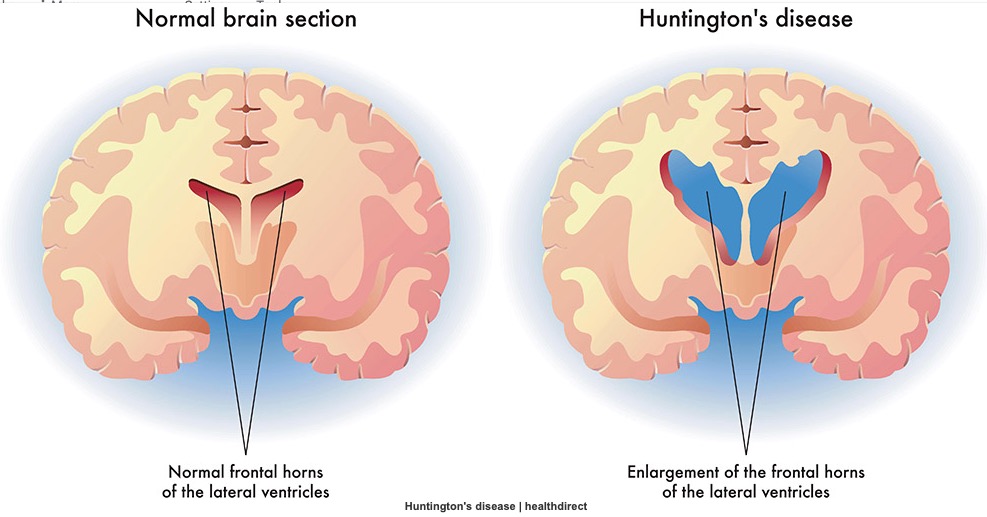
 亨廷顿氏病(HD)是一种遗传性的神经退行性疾病,通常在成年后表现出来,由HTT基因中的胞嘧啶-腺嘌呤(CAG)多谷胺增多引起。灰质损失开始于新纹状体,然后扩展到扣带回、前中央、前额叶区以及枕叶、顶叶和颞叶皮层,基底神经节的萎缩率最为明显。这种广泛的变性导致了三方面的进行性症状,包括运动功能障碍、认知障碍和神经精神障碍,如淡漠。
亨廷顿氏病(HD)是一种遗传性的神经退行性疾病,通常在成年后表现出来,由HTT基因中的胞嘧啶-腺嘌呤(CAG)多谷胺增多引起。灰质损失开始于新纹状体,然后扩展到扣带回、前中央、前额叶区以及枕叶、顶叶和颞叶皮层,基底神经节的萎缩率最为明显。这种广泛的变性导致了三方面的进行性症状,包括运动功能障碍、认知障碍和神经精神障碍,如淡漠。
淡漠是HD最常见的神经精神特征,在运动前表现和运动表现的HD患者中的发病率为46%-76%。因此漠对患者和护理人员的生活质量构成了重大负担,影响了自主性和社会生活。
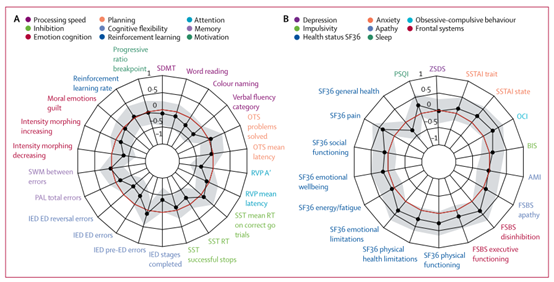
此外,与其他常见的HD神经精神症状(如抑郁症)不同,淡漠已被证明能密切反映认知和功能衰退的疾病进展,尽管这类报道不多。当考虑到HD淡漠的潜在大脑相关因素时,最近的研究显示,淡漠是由认知和边缘区域的皮质下和皮质区域调控。特别是较高的冷漠程度与各种成像模式下广泛的神经生物学变化有关,包括灰质体积(GMV)萎缩、功能连接减少和白质微结构受损。虽然这种横断面研究揭示了HD淡漠症的潜在治疗目标,但它们在描述一种进行性神经退行性疾病的纵向变化方面,适用性有限。
目前的研究很少研究HD淡漠的发展。同时,尽管有纵向研究,但这些研究缺乏神经影像学的数据。因此,在全脑水平上进行纵向分析,以确定皮层下和皮层水平的萎缩是否会在淡漠症出现之前出现,从而预测淡漠症的出现,是至关重要的。
这些特定的大脑改变模式反过来可以作为有针对性的生物标志物,辨别哪些人更容易随着疾病的发展而形成更多的神经精神临床特征。因此,这种个人层面的疾病特征区分将为早期干预提供机会,利用更加个性化的预防和治疗方案。
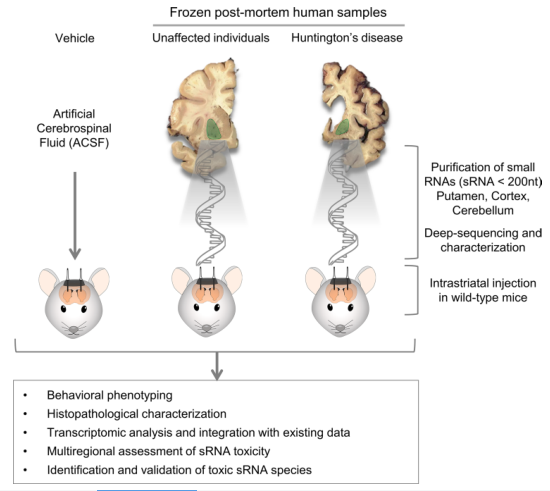
藉此,巴塞罗那大学的Audrey E. De Paepe等人探究了: 在整个HD过程中,GMV的变化与淡漠之间的关系。
首先,他们在全脑水平上进行了纵向的体素形态测量(VBM),以确定GMV萎缩可能描述两个时间点上淡漠严重程度变化的区域。
其核心假设:随着时间的推移,GMV的更大损失将与淡漠严重程度的更大增加有关。
他们发现,右侧MCC(middle cingulate cortex)的GMV萎缩与冷漠严重程度的增加有关,但与抑郁症或执行功能障碍无关。
另外,基线时MCC体积的敏感性,也能成功地预测冷漠的纵向严重程度和进展。
具体来说:MCC的体积较小可以预测那些更有可能发展为冷漠症的个体。推而广之,最初的MCC体积还为执行功能减退的预后提供信息。
原文出处:
De Paepe AE, Ara A, Garcia‐Gorro C, et al. Gray Matter Vulnerabilities Predict Longitudinal Development of Apathy in Huntington’s Disease. _Mov Disord_. May 2021:mds.28638. doi:10.1002/mds.28638.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Disord#
112
#Dis#
102
#亨廷顿病#
88
#亨廷顿#
97
学习
98
已读已读已读已读,学习学习学习学习学习,受益匪浅
100