例1
【一般资料】
患者女性,41岁
【主诉】
因发作性右上肢无力3天入院。
【现病史】
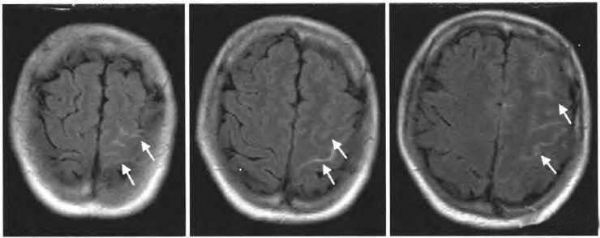
患者3天前劳累后出现发作性右上肢无力,表现为右手不能屈伸,右上肢不能抬举,持续约2~3min后症状缓解,共发作1次,无头痛、呕吐,无视物异常、言语不利,无肢体麻木感。遂就诊于当地医院,行头颅CT检查显示左侧额叶脑沟异常信号,头颅MRI检查显示左侧额叶脑沟T1WI高信号表现(图1),提示存在蛛网膜下腔出血,收入病房。
【体格检查】
内科体检未见异常。神经系统体检:意识清楚,精神可,言语流利,高级神经功能检查正常,脑神经检查正常。四肢肌力V级,肌张力正常,腱反射正常,双侧病理征未引出。感觉及共济运动检查正常。颈部稍抵抗,克尼格征(-),布鲁金斯征(-)。
【既往史】
既往体健,个人史、家族史无特殊
【辅助检查】
入院后检查三大常规、生化全项、出凝血机制、心电图及脑电图均正常。
【初步诊断】
患者蛛网膜下腔出血诊断明确,
【治疗】
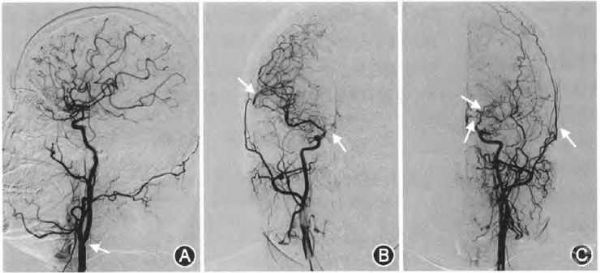
后行全脑血管造影,考虑烟雾病,其供血区主要由左侧颈外动脉(通过脑膜中动脉、颞浅动脉)、左侧大脑后动脉(通过软脑膜动脉)、左后交通动脉进行代偿。左椎动脉V1段闭塞,通过甲状颈干、颈升动脉及其他肌支吻合,其远端浅淡显影(图2)。
例2
【一般资料】
患者男性,54岁
【主诉】
因发作性言语表达困难、右手指麻木8天入院
【现病史】
患者8天前无明显诱因出现言语表达困难,表现为讲话不能,可以理解他人言语,持续1~2min后症状改善,后出现右手中指及食指指尖至指根的麻木症状,持续4~5min后症状完全缓解,无其他不适。患者就诊行头颅CT检查未见明显异常,诊断“短暂性脑缺血发作”,给予“拜阿司匹林、阿托伐他汀”药物治疗。1天前患者再次出现发作性言语表达困难、右手指麻木症状,言语表达困难症状同前,持续1min后症状缓解,出现右手食指及拇指指尖至指根的麻木症状,持续2~3min后症状改善。为明确诊治收入病房。
【体格检查】
内科体检未见异常。意识清楚,精神可,言语流利,高级神经功能检查正常。脑神经检查正常。四肢肌力5级,肌张力正常,腱反射正常,左侧巴宾斯基征可疑阳性,右侧病理征未引出。感觉及共济运动检查正常。颈软,克尼格征(-),布鲁金斯征(-)。
【既往史】
既往体健
【个人史】
吸烟平均10支/d×30年,偶有饮酒。家族史无特殊。
【辅助检查】
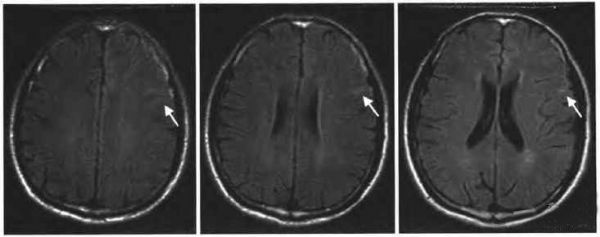
入院后检查三大常规、生化全项、出凝血机制、心电图及脑电图均正常。进一步完善MRI检查发现,头颈MRA+头颅MRI示:符合头颈部动脉硬化MRA表现;右侧大脑中动脉未见明确显示,考虑闭塞;左侧大脑中动脉M1段血流信号弱;左侧大脑前动脉A2-3段显示欠佳,多发狭窄;左侧大脑后动脉P3段局部狭窄;多发腔隙性脑梗死;左侧额叶局部脑沟异常信号,不除外蛛网膜下腔出血(图3)。
【治疗】
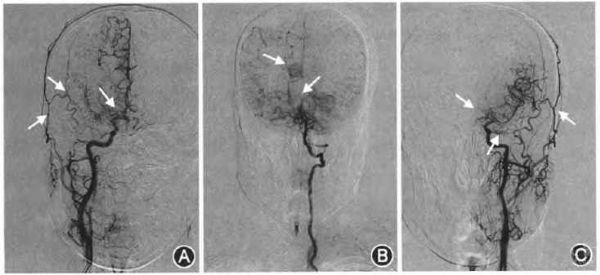
为进一步明确诊断,进行腰椎穿刺术检查,脑脊液分析示:外观微红色微浊无凝块,潘迪试验(+),蛋白定量0.52g/L,红细胞计数1760×10^6/L,明确蛛网膜下腔出血诊断。为查找蛛网膜下腔出血的病因,进行全脑血管造影术检查,考虑烟雾病可能(图4)。
【讨论】
脑底异常血管网病又称烟雾病,是以脑血管造影发现双侧颈内动脉虹吸部及大脑前、中动脉起始部严重狭窄或闭塞,颅底软脑膜、穿通动脉等小血管代偿增生形成脑底异常血管网为特征的一种慢性脑血管闭塞性疾病。随着影像学技术的发展,越来越多的烟雾病被发现。烟雾病起病年龄范围2~65岁,以儿童和青少年多见。有10~14岁和40岁左右两个发病年龄高峰。临床症状主要包括缺血性和出血性两组。10岁以下儿童患者以缺血型为主,表现为反复发生的短暂性脑缺血发作或脑梗死,可出现运动、意识、语言和感觉障碍。文献报道成人出血型烟雾病以脑出血及脑室出血为主,且主要表现为突发头痛、意识障碍、失语或肢体无力等,也有少数病例表现为自发性蛛网膜下腔出血。我们报道的2例成人患者临床表现为TFNE,其中1例表现为类似短暂性脑缺血发作的TFNE阴性症状,1例表现为扩散性感觉异常的TFNE阳性症状,2例患者均行头颅MRI检查发现脑沟内异常信号,考虑为蛛网膜下腔出血。短暂性局灶性神经系统发作在CAA患者中逐渐被认识,并且研究报道TFNE主要见于cSAH或皮质表面铁沉积(cSS)的患者,cSAH是位于大脑凸面的局灶性蛛网膜下腔出血,通常局限在相邻的几个脑沟内,多不伴有脑底面的蛛网膜下腔出血。2例患者均进行脑血管造影证实为烟雾病。目前关于cSAH导致TFNE的机制尚不确定,蛛网膜下腔出血后血液成分刺激所致的皮质播散性抑制、局灶性癫痫放电以及局部血管痉挛被认为是可能的机制。烟雾病所致的cSAH的病因考虑与代偿的皮质异常小血管的破裂有关。对表现为TFNE的烟雾病患者进行自身抗体检测,可能会有β淀粉样蛋白表达量的明显升高。通过复习以上文献报道,对我们临床工作的启示有以下几点:①需警惕表现为类似短暂性脑缺血发作的患者有可能为出血;②TFNE不仅仅是CAA患者的特征性症状之一,而更应该是cSAH的特征性临床表现;③对于不同年龄层的cSAH患者,应进一步查找病因;④明确cSAH病因,有助于评估患者长期预后,CAA患者预后相对较差,而脑动脉狭窄或闭塞的患者预后良好。关于烟雾病所致cSAH的发病机制尚不明确,且临床报道较少,需进一步研究及总结,以制定相应治疗策略及评估患者预后。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#短暂性#
78
#局灶性#
0
#神经系统#
65
阅
116
学习了.谢谢分享.
113
了解一下.谢谢分享!
96
学了
88