JCEM:1型糖尿病成人椎体骨折的患病率
2022-02-19 MedSci原创 MedSci原创
研究人员使用mABQ方法评估的脊椎骨折评估结果并未证实1型糖尿病控制相对良好的男性和女性的脊椎骨折患病率有所增加。
据报道,在1型糖尿病的年轻患者中,脊椎骨折的患病率高达24%。如果这种高患病率得到证实,1型糖尿病患者可以从预防性脊椎骨折的筛查工作中受益。

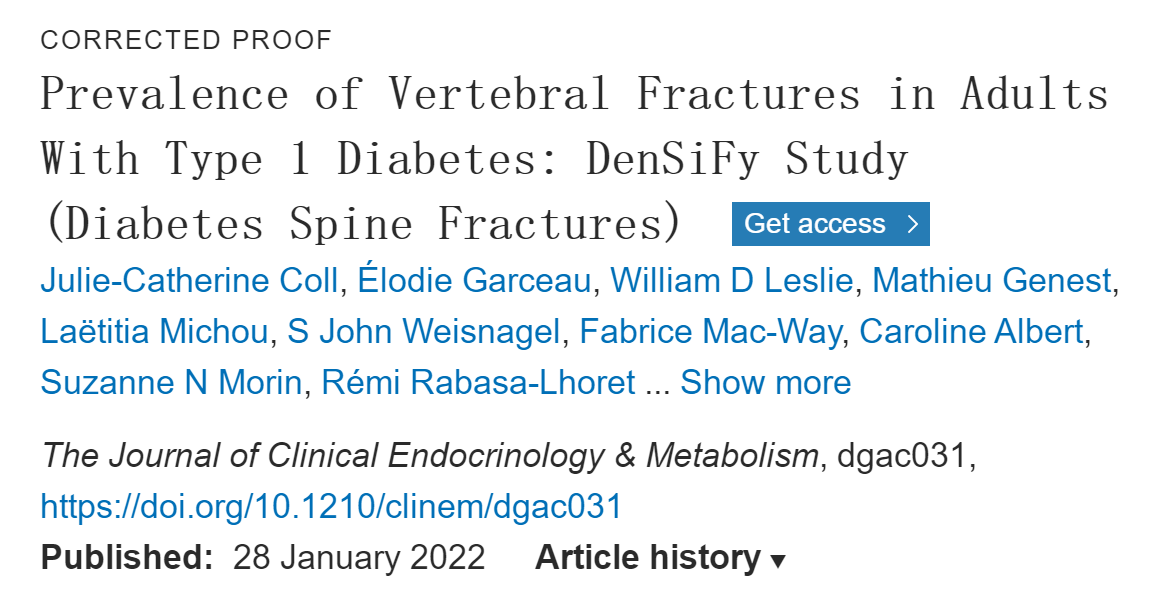
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在比较1型糖尿病成人和非糖尿病对照者之间的脊椎骨折的患病率。
这项横断面研究纳入了来自2个三级医疗中心门诊就诊的127名1型糖尿病成人和65名年龄、性别和BMI大小相匹配的对照者。研究人员通过双能X线骨密度仪(DXA)进行的椎体骨折评估,用于常见的脊椎骨折。研究人员采用了改进的基于算法的定性(mABQ)方法进行分析。研究人员通过DXA评估骨矿物质密度(BMD)和骨小梁评分(TBS)。此外,研究人员在一组参与者中测量了血清骨转换标志物和硬化蛋白。

1型糖尿病参与者(70名女性,57名男性)的平均年龄为42.8±14.8岁,中位糖尿病病程为25.8(15.8-34.4)年,平均BMI为26.6±5.4kg/m2,过去3年的平均HbA1c为7.5±0.9%。对照组(35名女性,30名男性)的平均年龄为42.2±15.9岁,平均BMI为26.1±5.1kg/m2。两组之间的脊椎骨折患病率相当(2.4% vs. 3.1%,P=0.99)。1型糖尿病患者与对照组的TBS、全髋关节和股骨颈的BMD以及骨形成和再吸收标志物均较低,而硬化蛋白水平相似。
由此可见,研究人员使用mABQ方法评估的脊椎骨折评估结果并未证实1型糖尿病控制相对良好的男性和女性的脊椎骨折患病率有所增加。
原始出处:
Julie-Catherine Coll.et al.Prevalence of Vertebral Fractures in Adults With Type 1 Diabetes: DenSiFy Study (Diabetes Spine Fractures).JCEM.2022.https://academic.oup.com/jcem/advance-article-abstract/doi/10.1210/clinem/dgac031/6517001?redirectedFrom=fulltext&login=false
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCE#
56
#JCEM#
51
#椎体骨折#
57
学习
76
#患病率#
51
#椎体#
103
学习
58
交叉知识,学习学习
61