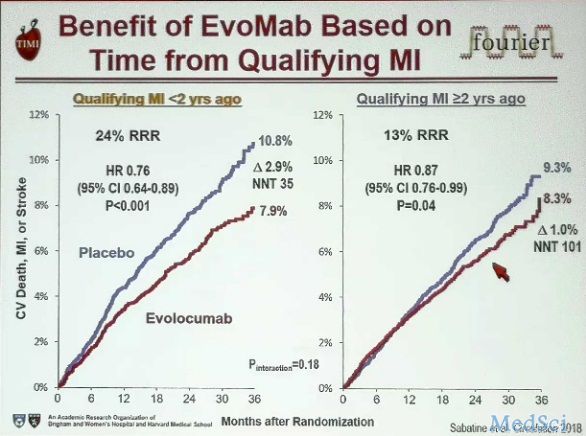
2018AHA热点持续升温!PCSK9抑制剂再添新证
2018-11-13 中国心血管健康联盟进阶学院 MedSci原创
AHA科学年会如火如荼的进行当中,PCSK9抑制剂作为本次大会讨论的热点之一,亦有众多精彩内容呈现!
AHA科学年会如火如荼的进行当中,PCSK9抑制剂作为本次大会讨论的热点之一,亦有众多精彩内容呈现!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PCS#
73
#PCSK9抑制#
60
#Csk#
70
#抑制剂#
49
#AHA#
80