诺华与盖茨基金会组成联盟开发隐孢子虫病药物
2018-02-25 MedSci MedSci原创
诺华与比尔&梅林达盖茨基金会已组成联盟,推动诺华制药候选化合物KDU731用于治疗隐孢子虫病。
诺华与比尔&梅林达盖茨基金会已组成联盟,推动诺华制药候选化合物KDU731用于治疗隐孢子虫病。
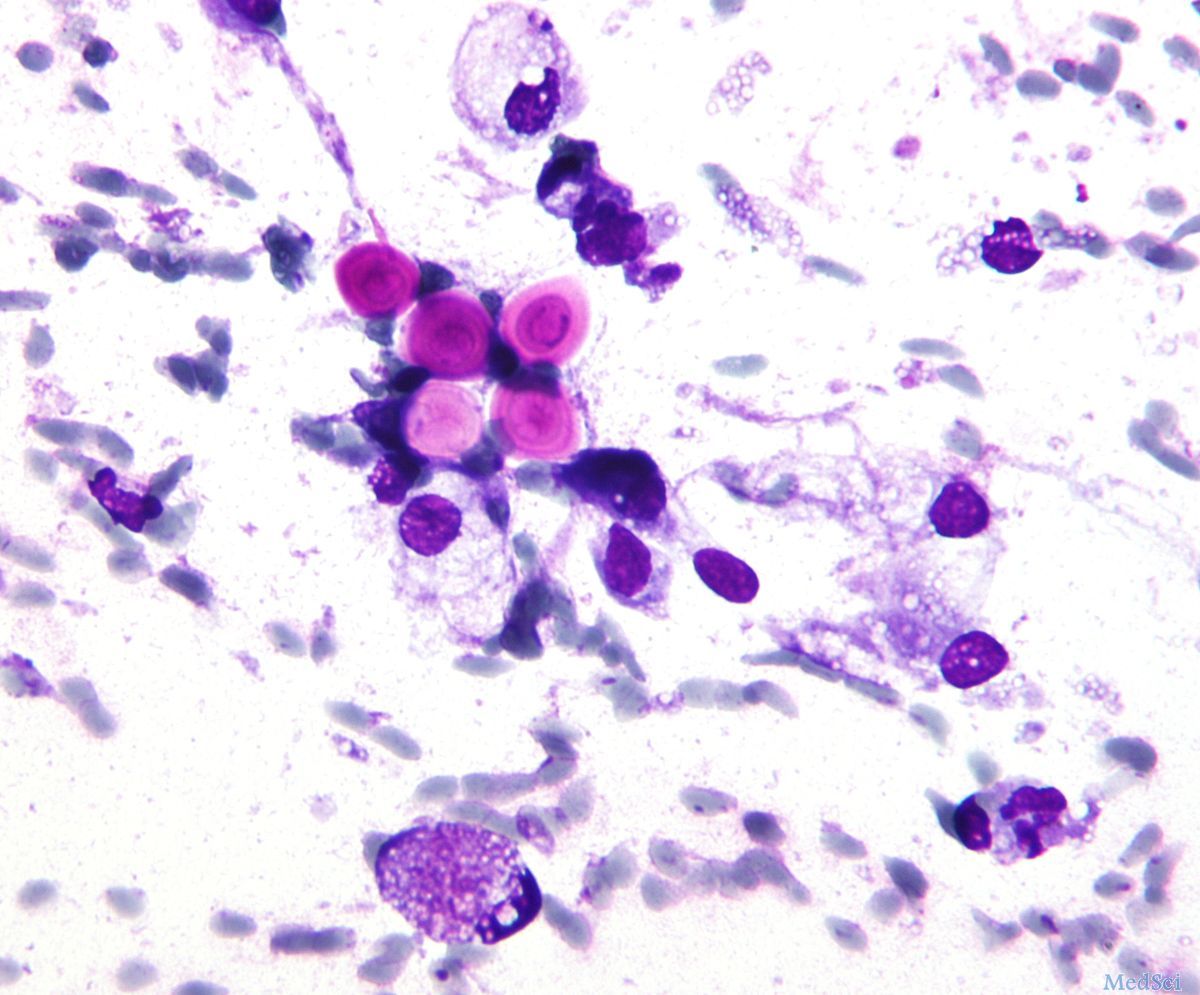
腹泻是全球儿童死亡的主要原因之一,每年约有525,000人死亡,隐孢子虫病是2岁以下儿童感染性腹泻的第二大原因。隐孢子虫病(Cryptosporidiosis)是由单细胞寄生虫隐孢子虫(Cryptosporidium)造成的脊椎动物肠道疾病,是导致人腹泻的主要原因之一。这是一类通过粪口途径传播的疾病,病原体通常寄生在小肠上皮细胞的带虫空泡内。免疫缺陷患者(如艾滋病病人)经常患有此类并发症,由于免疫功能的不完善,寄生虫还可能会进入病人的肝、肺、胰和胆囊等器官,造成更为严重的病理反应。隐孢子虫病是一种水源性疾病(waterborne disease),病原体在水中以卵囊(oocyte)形式存在并得以传播,对水中环境有较好的耐受性,因此饮用不洁净的水成为该病的主要患病原因。
对于隐孢子虫病急需新型的有效疗法,特别是在易感人群中。KDU731是一种隐孢子虫脂质激酶PI K(磷脂酰肌醇-4-OH激酶)抑制剂,已在临床前模型中被证明可有效治疗隐孢子虫感染,目前正在开展临床试验前的安全性研究。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/72818/novartis-medicines-cryptosporidiosis/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#盖茨基金会#
98
#诺华#
70
#联盟#
60
学习了
0