Toxicol Sci:肺部炎症诱发全身炎症、内皮功能障碍和胰岛素抵抗
2017-11-19 Emma MedSci原创
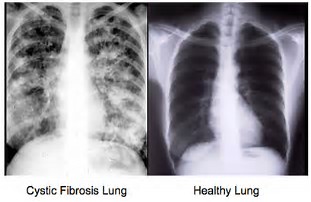
肺部不断暴露于周围的细微物质(PM2.5)等环境污染物,使其成为人体最常见的炎症部位之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#内皮功能障碍#
70
#胰岛#
70
#肺部炎症#
98
继续学习中谢谢
125
学习了谢谢分享
114
#功能障碍#
51
#内皮功能#
95
#全身炎症#
56
学习学习.继续关注
110
谢谢分享.学习了
103