NEJM:自发性咽后血肿-案例报道
2016-01-21 MedSci MedSci原创
http://www.nejm.org/doi/full/10.1056/NEJMicm1505596
男性,56岁,因咽喉肿痛、呼吸困难、仰卧位时伴有加重而到急诊室求诊。在出现这些症状前,其无外伤史。
经问诊,该男子既往有前列腺癌、高血压、高脂血症、深静脉血栓形成和中风病史。曾应用过的药物包括:华法林、抗高血压药和他汀类药物。
常规体格检查发现,其后口咽部有显著的轻微肿胀并伴有发热。
实验室检查显示白细胞计数正常,凝血酶原时间为120s和活化部分凝血活酶时间为127s。
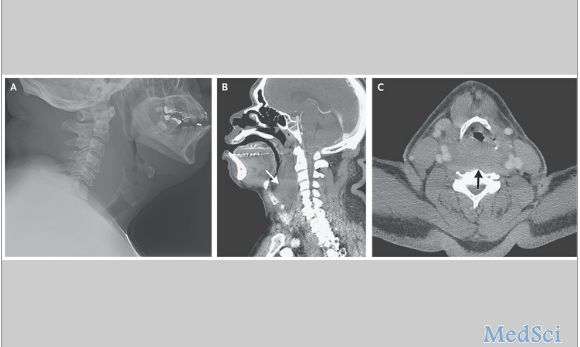
颈部的X线片显示软组织肿胀,压迫气道(如图A所示);在随后的颈部CT扫描检查中的显示的结果与X线片检查结果一致。会诊医师猜测着可能是应用抗凝药物引起的血肿(图B显示矢状位、图C为轴视图;箭头所指为血肿处)。
4天后,该男子的凝血功能障碍得到解决,症状减缓,顺利康复出院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好的病例
128
赞一个!好文章拜读了,认真学习了。
116
罕见
155
长见识
164
#血肿#
70
#自发性#
86