Nature:全球首例移植干细胞治疗帕金森的人体试验启动
2018-11-17 Tierna 生物探索
帕金森研究领域迎来新突破!据《Nature》杂志封面14日的报道,日本京都大学的科学家首次利用人类诱导多能干细胞(iPS细胞)制作的神经细胞对帕金森病患者进行移植治疗。据悉,该手术于上个月进行,是试验帕金森病新疗法的一个里程碑式的进步。
帕金森研究领域迎来新突破!据《Nature》杂志封面14日的报道,日本京都大学的科学家首次利用人类诱导多能干细胞(iPS细胞)制作的神经细胞对帕金森病患者进行移植治疗。据悉,该手术于上个月进行,是试验帕金森病新疗法的一个里程碑式的进步。
帕金森病是一种神经系统变性疾病,影响全球约2%的60岁以上人群,主要病理改变是脑部分泌多巴胺的神经细胞死亡,临床表现包括手脚震颤、身体僵硬、行动迟缓等,目前尚无根治方法。
去年8月,日本科学家Tetsuhiro Kikuchi在发表于《Nature》杂志的题为“Human iPS cell-derived dopaminergic neurons function in a primate Parkinson’s disease model”的文章中已经证明,多巴胺前体细胞能改善猴子帕金森病的症状。
当时,Takahashi团队将健康人群和帕金森患者的iPS细胞转化为能产生多巴胺的神经元。然后将这些细胞移植到猕猴帕金森模型中。结果显示,移植的脑细胞存活了至少两年,并与猴子的脑细胞形成了连接,被细胞治疗的猴子运动能力得到显着改善。
更令人惊喜的是,Takahashi的研究小组没有观察到移植细胞有发育成肿瘤的迹象——这是多能细胞治疗面临的一个最关键问题。并且,细胞移植也没有引发严重的免疫反应。
首批猴类模型显示积极结果后,很快,日本政府于今年7月批准了京都大学iPS细胞研究所提出的首个人体临床试验:将以所保存的健康捐赠者iPS细胞,培养约500万个可产生多巴胺的神经细胞,再将这些能分化成神经细胞的前体细胞移植到帕金森病患者脑部,以试验这种方法治疗帕金森病的有效性和安全性。
按计划,该临床试验将为7名患者进行移植。这7名患者都在50岁-60岁之间,患帕金森病均在5年以上,药物治疗效果不佳。
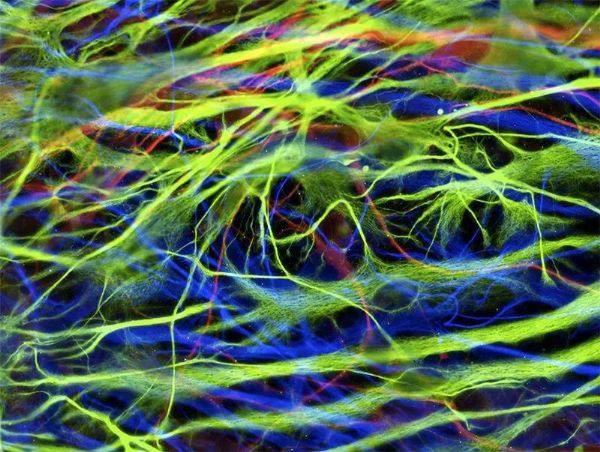
干细胞衍生的神经元。图片来源:Silvia Riccardi/SPL
10月,京都大学医院的神经外科医生Takayuki Kikuchi将240万多巴胺前体细胞植入一名患者的左脑。在三个小时的过程中,Kikuchi的团队将细胞沉积到12个多巴胺活动的中心部位。
研究人员表示,患者状况良好,到目前为止还没有重大的不良反应。该团队将观察他六个月,如果没有并发症发生,将会在他的右脑中植入另外240万个多巴胺前体细胞。
之后,该团队计划在2020年底前再治疗6名帕金森病患者,以测试该技术的安全性和有效性。
Kikuchi说,如果试验进展顺利,在证据足够的前提下,可在2023年根据日本药物审批制度将这一疗法出售给患者。
原始出处:‘Reprogrammed’ stem cells implanted into patient with Parkinson’s disease:A man in his 50s is the first of seven patients to receive the experimental therapy. Nature. 14 NOVEMBER 2018
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
74
#全球首例#
97
#人体试验#
87
#移植干细胞#
75
学习了,长知识
105
好
104
向日本科研人员致敬!!!
94
谢谢了,学习
98