Hypertension:动态血压监测对高血压诊断很重要,不服来PK!
2016-12-28 xing.T MedSci原创
在这项常规临床实践中的大型研究中,诊室血压将>40%的患者错误地划分为高血压患者。这个错误受年龄影响不大,但是在临近高血压和1级高血压患者中更加明显。这些发现进一步表明了在常规临床实践中通过动态血压监测来明确血压状态的重要性。
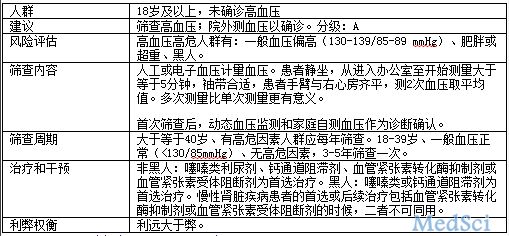
在高血压患者中诊所血压通常高于日间动态血压,但最近的一些研究对这一观点提出了质疑,并表明这种关系受年龄的影响较大。近日,心血管权威期刊Hypertension上发表一篇研究文章,研究人员采用西班牙动态血压监测队列为基础,在常规初级保健实践中104,639例横跨各个年龄段的成年高血压患者(诊室收缩压/舒张压≥140/90mmHg或进行抗高血压治疗 )中来评估年龄对诊所血压与日间动态血压之间差异的影响。
为了评估年龄、心血管变量和诊所血压对诊室-白天动态血压的差异的影响,研究人员建立了针对平均血压差异、白大衣性高血压(高诊室血压,而白天动态血压正常)和隐匿性高血压(诊室血压正常,高白天动态血压)的多变量回归模型。
研究人员发现在所有年龄段的大多数患者中,平均诊室血压值高于白天动态血压。大约有36.7%的患者为白大衣性高血压(高达50%的患者诊室收缩压达140-159mmHg)和3.9%的患者有隐匿性高血压(18%的患者诊室收缩压达130-139mmHg)。定量或分类血压的差异其中0.1%-1.7%的不同可以用年龄来解释(P<0.001)。心血管变量解释了额外的1.6%-3.4%的差异(P<0.001)。最后,诊所血压整体上解释了≥20%的差异(P<0.01)。
在这项常规临床实践中的大型研究中,诊室血压将>40%的患者错误地划分为高血压患者。这个错误受年龄影响不大,但是在临近高血压和1级高血压患者中更加明显。这些发现进一步表明了在常规临床实践中通过动态血压监测来明确血压状态的重要性。
原始出处:
José R. Banegas,et al. Clinic Versus Daytime Ambulatory Blood Pressure Difference in
Hypertensive Patients The Impact of Age and Clinic Blood Pressure. Hypertension.
December 27, 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TENS#
56
#动态血压监#
0
#PE#
61
#动态血压监测#
70
#Hypertension#
85
#动态血压#
64