Nanoscale:UTMD辅助PDT和基因治疗或可有效治疗三阴乳腺癌
2018-11-01 MedSci MedSci原创
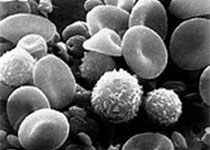
三阴乳腺癌(TNBC)是一种侵袭性乳腺癌,由于缺乏孕激素受体(PR)、雌激素受体(ER)和HER2的表达,TNBC的复发率和整体存活率均差于其他乳腺癌亚型。为了提高TNBC的治疗效果,我们开发了一种新型多功能阳离子卟啉接枝脂质(CPGL)微泡,载有HIF1αsiRNA(siHIF@CpMB)。 由于CPGL的两亲结构,它可以与常规脂质自组装成微泡(MB),卟啉基团可以用作光动力疗法(PDT)
三阴乳腺癌(TNBC)是一种侵袭性乳腺癌,由于缺乏孕激素受体(PR)、雌激素受体(ER)和HER2的表达,TNBC的复发率和整体存活率均差于其他乳腺癌亚型。为了提高TNBC的治疗效果,我们开发了一种新型多功能阳离子卟啉接枝脂质(CPGL)微泡,载有HIF1αsiRNA(siHIF@CpMB)。
由于CPGL的两亲结构,它可以与常规脂质自组装成微泡(MB),卟啉基团可以用作光动力疗法(PDT)的光敏剂,而氨基可以通过静电吸附吸附HIF1αsiRNA(siHIF)。这种MB具有非常高的药物负载含量和较少的过早药物释放。通过实时US成像(3-12 MHz)可以轻松监控MB的分布。此外,借助超声靶向微泡破坏(UTMD),siHIF@CpMBs可以有效地原位转化为纳米粒子,通过空化效应促进卟啉和siRNA在肿瘤部位的积聚。HIF1αsiRNA下调HIF1α的表达水平,其由常见的缺氧肿瘤环境或ROS(由PDT产生)诱导,增强PDT功效并部分抑制肿瘤进展。
因此,UTMD辅助PDT和基因治疗的组合是治疗TNBC的有效策略。
原始出处:
Sun S, Xu Y, et al., Ultrasound-targeted photodynamic and gene dual therapy for effectively inhibiting triple negative breast cancer by cationic porphyrin lipid microbubbles loaded with HIF1α-siRNA. Nanoscale. 2018 Oct 22. doi: 10.1039/c8nr03074j.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#scale#
115
#TMD#
122
#PDT#
189
#有效治疗#
101