JCLA:肿瘤坏死因子的功能性变体β基因在颞下颌紊乱的影响量
2019-06-01 不详 网络
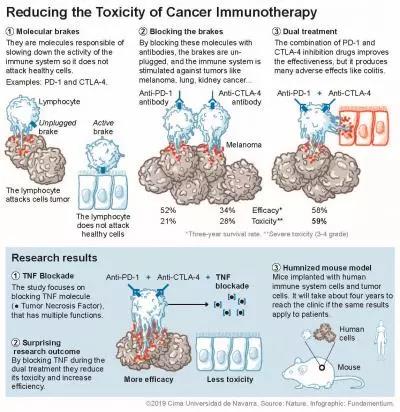
颞下颌关节紊乱症(TMD)是一组引起慢性口腔颌面部疼痛的疾病。肿瘤坏死因子β(TNFβ)是一种促炎细胞因子,参与炎症过程包括组织和维护的各个方面,以及在炎症细胞的排列。本研究的目的是在土耳其的队中列评估肿瘤坏死因子检测β+ 252 a / G (rs909253)变体和易感性之间的相关性。
颞下颌关节紊乱症(TMD)是一组引起慢性口腔颌面部疼痛的疾病。肿瘤坏死因子β(TNFβ)是一种促炎细胞因子,参与炎症过程包括组织和维护的各个方面,以及在炎症细胞的排列。本研究的目的是在土耳其的队中列评估肿瘤坏死因子检测β+ 252 a / G (rs909253)变体和易感性之间的相关性。
研究包括104例TMD患者(26名男性,78名女性)和126名健康对照组(44名男性,82名女性)。肿瘤坏死因子检测β+ 252 a / G变异分析基于聚合酶链反应检测限制片段长度多态性(PCR RFLP)。
研究发信啊,在病人和对照组没有偏离TNFβ+ 252A/G变体。患者组和对照组的肿瘤坏死因子β+ 252 / G变体之间分别有显著差异基因型和等位基因频率
(P = 0.010, 0.015)。与健康对照组相比,发现TMD患者一个显著增加肿瘤坏死因子β+ 252 AG基因型和G等位基因频率。具有GG基因型和G等位基因的个体发生TMD的风险增加。当按AA基因型与AG+GG基因型与对照组比较时,观察到有统计学意义的相关性(P = 0.002,或:2.23,95% CI:1.31‐3.82)。肿瘤坏死因子β+ 252 A/G 基因型分布与咀嚼问题(P = 0.046)。
总之,我们的研究结果提供的证据表明,肿瘤坏死因子量β252 A/G变异可能导致土耳其研究队列中TMD的发展。需要进一步的研究来证实这一观察结果。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#功能性#
128
#颞下颌#
125
#颞下#
110
#下颌#
91
#坏死#
96
#肿瘤坏死因子#
96