科学家解析甲肝病毒与中和性抗体复合物三维结构
2017-01-20 彭科峰 科学网
日前,中科院生物物理所饶子和团队和牛津大学科研人员合作,解析了甲肝病毒与其中和性抗体Fab复合物精细三维结构,通过病毒学和细胞生物学实验证明:该抗体不仅能够阻断HAV与其受体TIM-1分子的相互作用,还干扰了HAV病毒正常的脱衣壳过程,揭示了一种“Receptor Mimic”的中和机制,为抗病毒药物研发提供重要信息。相关成果发布于《美国科学院院刊》。 全球每年仍然有140万甲型肝炎病毒
日前,中科院生物物理所饶子和团队和牛津大学科研人员合作,解析了甲肝病毒与其中和性抗体Fab复合物精细三维结构,通过病毒学和细胞生物学实验证明:该抗体不仅能够阻断HAV与其受体TIM-1分子的相互作用,还干扰了HAV病毒正常的脱衣壳过程,揭示了一种“Receptor Mimic”的中和机制,为抗病毒药物研发提供重要信息。相关成果发布于《美国科学院院刊》。
全球每年仍然有140万甲型肝炎病毒(HAV)感染病例,主要爆发于发展中国家。2015年饶子和研究团队解析了HAV全病毒颗粒的晶体结构,揭示了HAV独有的结构特性、极强的稳定性和小RNA病毒的进化关系。然而,HAV的受体结合位点以及具有极强稳定性的病毒是如何发生脱衣壳的分子机制还是不清楚。
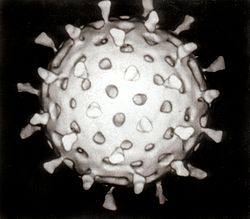
科研人员结合低温冷冻电镜技术、X射线晶体学和病毒学技术,解析了HAV病毒实心颗粒(3.4埃,约4500颗粒)、HAV病毒空心颗粒(3.9埃,约4000颗粒)和HAV病毒实心颗粒与抗体复合物(4.1埃,约1500颗粒)以及中和性抗体R10 Fab的晶体结构,确定了精细抗原表位,且该抗原表位在6株人类甲型肝炎病毒均高度保守。他们结合功能性数据表明:R10能够阻断HAV分子与TIM-1分子的结合和干扰HAV脱衣壳的特性,从结构和功能上提出了一种“受体模拟”的中和机制。
该研究对于阐述HAV病毒的受体结合位点和脱衣壳过程具有重要意义,为抗HAV病毒药物的研发提供理论指导和新方向。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#中和性抗体#
64
#三维结构#
47
#解析#
51
#复合物#
51
#甲肝#
50