BJC:新的测试将癌症复发消灭在萌芽状态!
2017-07-07 sunshine2015 来宝网
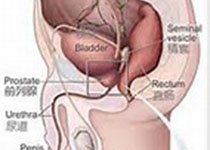
根据英国“癌症杂志”今日公布的研究,科学家们已经设计了一种简单的测试方法,对现有方法进行膀胱癌的早期准确预警。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,谢谢分享
99
学习了,谢谢分享
110
#癌症复发#
65
学习谢谢分享
100
这个观点独特
111