JAMA Netw Open:有妊娠糖尿病史的女性,每天饮酒 5.0 至 14.9 克可将 2 型糖尿病风险降低一半?
2021-09-15 MedSci原创 MedSci原创
2型糖尿病(T2DM)是一种慢性代谢疾病,占糖尿病患者90%以上,预防2型糖尿病是全球公共卫生工作重点。先前研究显示,与没有妊娠糖尿病史的女性相比,有妊娠糖尿病史的女性患2型糖尿病的风险增加7倍以上。
2型糖尿病(T2DM)是一种慢性代谢疾病,占糖尿病患者90%以上,预防2型糖尿病是全球公共卫生工作重点。先前研究显示,与没有妊娠糖尿病史的女性相比,有妊娠糖尿病史的女性患2型糖尿病的风险增加7倍以上。
pixabay
目前认为有不少生活方式都是引起T2DM的重要因素,特别是可改变的饮食和生活方式因素,其中包括肥胖症和超重(BMI高于25)、身体活动量不足、不健康的饮食、压力过大以及城市化的生活等,特别是轻度至中度饮酒。
近日,发表在JAMA Netw Open杂志的一项研究显示,在有妊娠糖尿病史的女性中,与不饮酒女性相比,每天饮酒 5.0 至 14.9 克与 2 型糖尿病风险降低 55% 相关。

这项队列研究包括护士健康研究II队列中报告有妊娠糖尿病史的妇女,并从1991年1月1日至2017年12月31日进行随访,作为糖尿病和妇女健康研究的一部分。数据分析是在2020年至2021年。研究人员评估了患有妊娠糖尿病史的女性饮酒与 2 型糖尿病风险之间的关联。
结果显示,共纳入4740名女性,平均年龄为38.2岁,随访中位时间为24年,共随访78328人年。在此期间,共有897例确诊2型糖尿病。在调整了饮食和生活方式因素后,与不饮酒的女性相比,饮酒5.0至14.9克/天与2型糖尿病发病风险下降有关;饮酒0.1至4.9克/天或15.0克/天或以上(最多74.2克/天)与2型糖尿病风险没有关联。
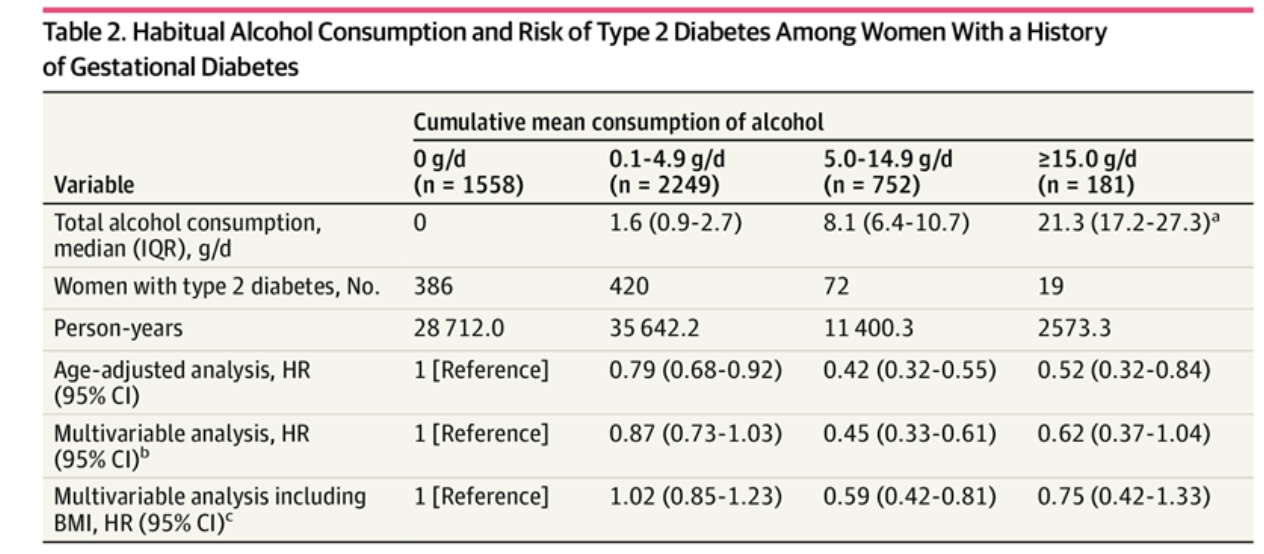
有妊娠糖尿病史的女性的习惯性饮酒和 2 型糖尿病风险
在调整了体重指数后,报告饮酒量为5.0-14.9 g/d的女性患2型糖尿病的风险降低了41%,饮酒量为0.1-4.9 g/d和饮酒量为15.0 g/d或以上仍与2型糖尿病风险无关,但结果有所削弱。
总之,在这项队列研究中,观察到有妊娠糖尿病史的女性每天饮酒 5.0 至 14.9 克与患 2 型糖尿病的风险呈负相关。在考虑对有妊娠糖尿病史的个体女性的临床建议时,应结合饮酒的其他已知风险和益处来解释研究结果。
原始出处
Stefanie N. Hinkle, PhD; Wei Bao, MD, PhD; Jing Wu, MD, MSc; et al.Association of Habitual Alcohol Consumption With Long-term Risk of Type 2 Diabetes Among Women With a History of Gestational Diabetes.JAMA Netw Open. 2021;4(9):e2124669. doi:10.1001/jamanetworkopen.2021.24669
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
54
#NET#
62
#风险降低#
135
有冲突了
87
看来适度喝酒也并非坏事
93
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
102
谢谢MedSci提供最新的资讯
82
有意思
77