急性小肠病变丨CT表现
2020-05-08 花人青 熊猫放射
许多病变可以诱发小肠急性病理改变,其特征性的CT表现较少。特定的临床信息,包括疾病的时程和发作时间,患者的危险因素以及任何最近的药物或放射疗法,通常有助于提高鉴别诊断。小肠相关疾病非常广泛,影响小肠的
许多病变可以诱发小肠急性病理改变,其特征性的CT表现较少。特定的临床信息,包括疾病的时程和发作时间,患者的危险因素以及任何最近的药物或放射疗法,通常有助于提高鉴别诊断。小肠相关疾病非常广泛,影响小肠的肿瘤性和感染性疾病可能会突然出现症状,在此不作具体讨论。
主要内容:
◆ 局部或广泛影响小肠的血管疾病,包括血栓栓塞和血流灌注不足现象,以及一系列的脉管炎。
◆ 小肠疾病的医源性原因,包括血管紧张素转化酶(ACE)抑制剂引起的血管性水肿,以及化学疗法和放射疗法相关的疾病形式。
◆ 影响小肠的自身免疫性、遗传性疾病,包括系统性红斑狼疮和遗传性C1酯酶抑制剂缺乏症。
知识点
◆ 在腹盆部的CT增强图像上,“靶征”或“双环征”代表分层的肠壁,内部黏膜层和外部的固有肌层/浆膜层明显强化,中间层为低密度的黏膜下水肿。
◆ 小肠扩张(直径>3 cm)并肠壁纸样变薄,提示由于血栓栓塞性疾病导致的急性血管功能损害。
◆ CT上在某个位置的一小段小肠上两个点的机械性梗阻可能会形成扭曲的C或U形结构,通常为闭环小肠梗阻(closed-loop small-bowel obstruction)的典型表现。
◆ 年轻患者,小肠的病变部分分布不典型(例如十二指肠内多个血管区域的斑片状分布),并且当类似情况伴有全身性感染时,应考虑血管炎(Vasculitis)。
◆ ACE抑制剂引起的血管性水肿CT表现包括:肠壁环形增厚(最常受累的是空肠),壁分层,肠管变直,肠系膜水肿和腹水。
小肠的急性疾病与结肠的不同,部分原因是小肠独特的血管供应和生理功能。非局部性急性腹痛通常是疾病首先出现的临床表现,急诊就诊时会使用增强CT进行初步影像学检查。
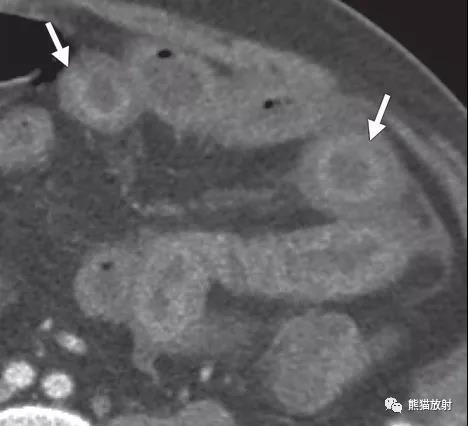
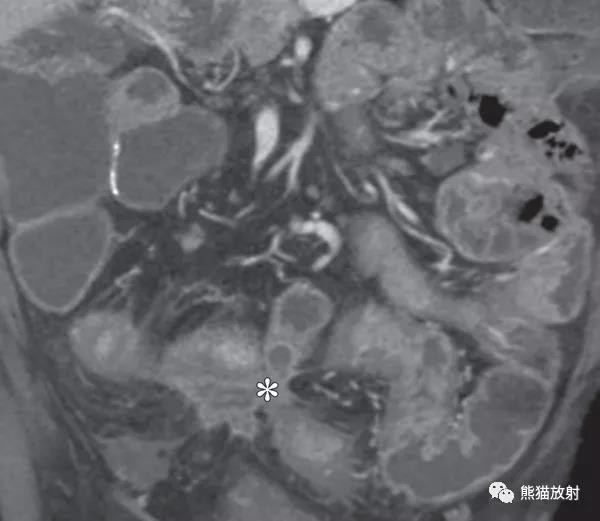
小肠弥漫性或局限性急性疾病的CT征象无特异性,最常见的表现是肠壁分层和周围肠壁增厚(下图)。
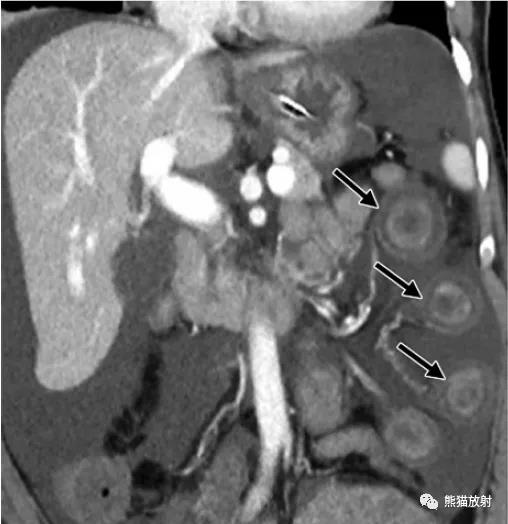
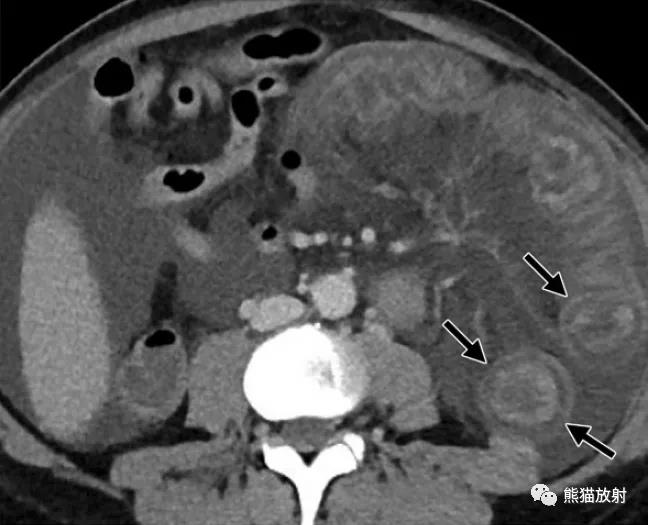
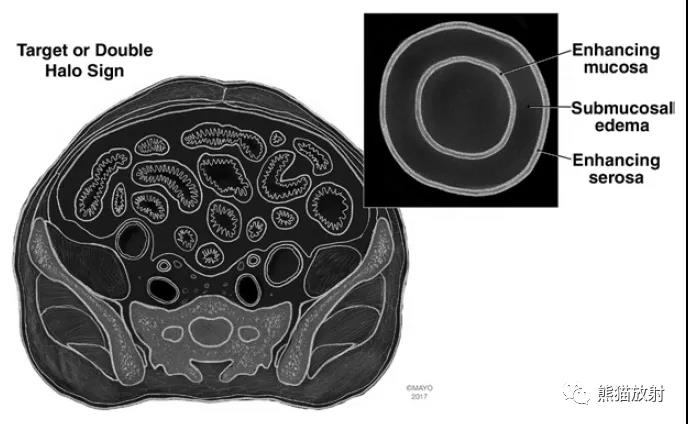
靶征或双环征(Target or double halo sign)
冠状CT增强动脉期示一名59岁末期肾脏疾病患者,轴位CT增强静脉期为小血管缺血的女性患者。双环:内、外环为强化的黏膜和固有肌层/浆膜(箭头),中间层为低密度的黏膜下水肿。注意由于空肠缺血性改变引起的反应性腹水和肠系膜水肿。插图显示“双环征”,轴位视图:强化的内侧黏膜层和外侧的固有肌层/浆膜层,中间为黏膜下水肿。
血管原因导致的小肠病变
Vascular Causes of Small-Bowel Disorders
急性肠系膜缺血 Acute Mesenteric Ischemia
◆ 急性动脉栓塞 Acute Arterial Embolism
◆ 急性静脉栓塞 Acute Venous Thrombosis
◆ 其它因素 Other Disease Considerations

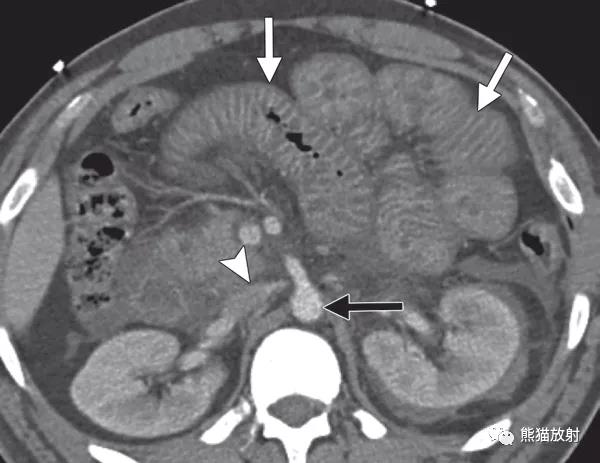
肠系膜上动脉(SMA)血栓形成而导致的急性肠系膜缺血。62岁男性,严重腹痛,增强CT显示SMA起始部血栓形成(箭),无强化;部分空肠扩张,肠壁薄如纸片,腔内积液呈高密度分层(箭头),提示出血性梗死。
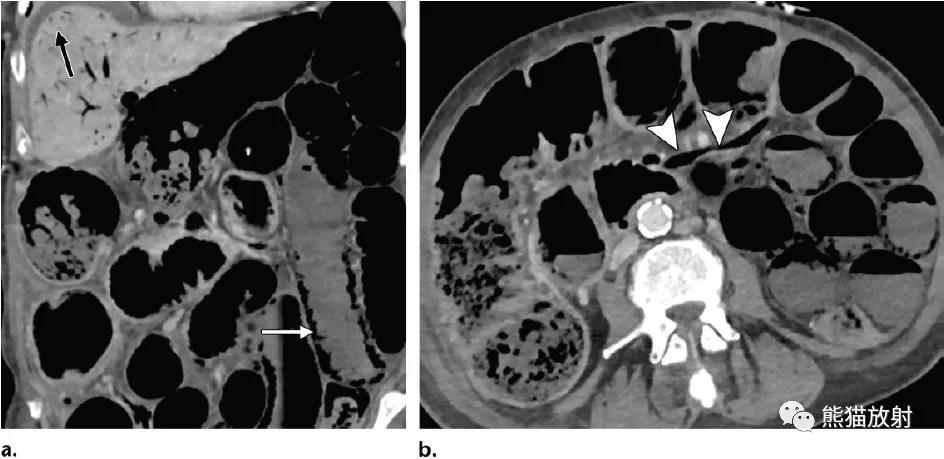
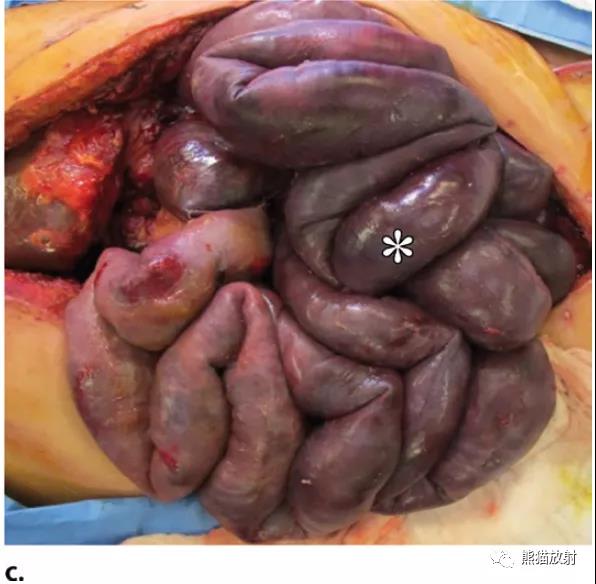
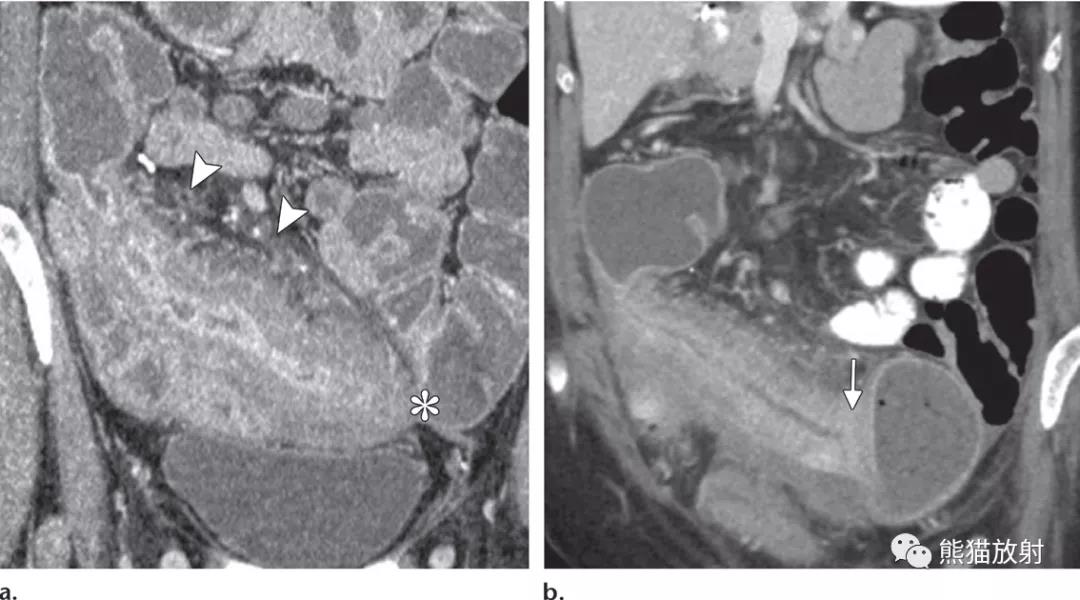
急性肠系膜缺血伴小肠梗死。72岁女性,弥漫性腹痛和低血压。冠状和轴位增强CT显示多个扩张的肠管,壁薄并强化程度减低,弥漫性气肿(a白箭)和门静脉气体(a黑箭)。注意空肠肠系膜静脉分支中的气体(b箭头)。剖腹手术照片显示广泛的小肠坏死(*)。
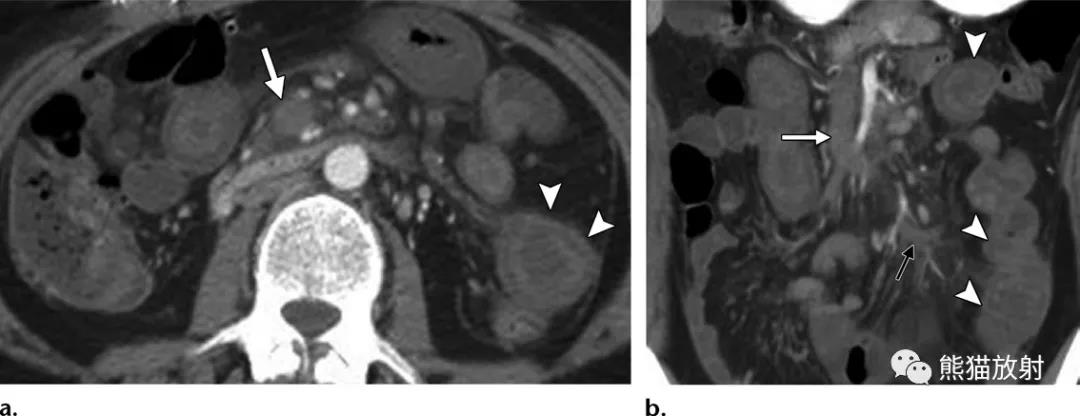
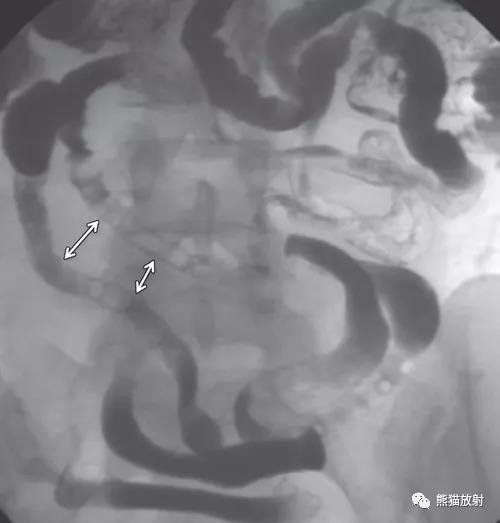
急性肠系膜静脉缺血。43岁妇女,急性狼疮性抗凝物检测结果阳性,急性腹痛。增强CT显示肠系膜上静脉(白箭)及其空肠分支内有闭塞性血栓,并有数个厚壁空肠(箭头),呈靶征,强化程度较低。注意肠系膜水肿和积液(b黑箭),这是肠系膜静脉缺血的常见特征。
急性肠系膜静脉缺血。53岁男性,肝硬化,腹胀、腹痛。口服造影剂、增强CT显示肠系膜上静脉闭塞性血栓(a箭),弥漫性小肠壁增厚,肠系膜水肿(箭头)和积液。


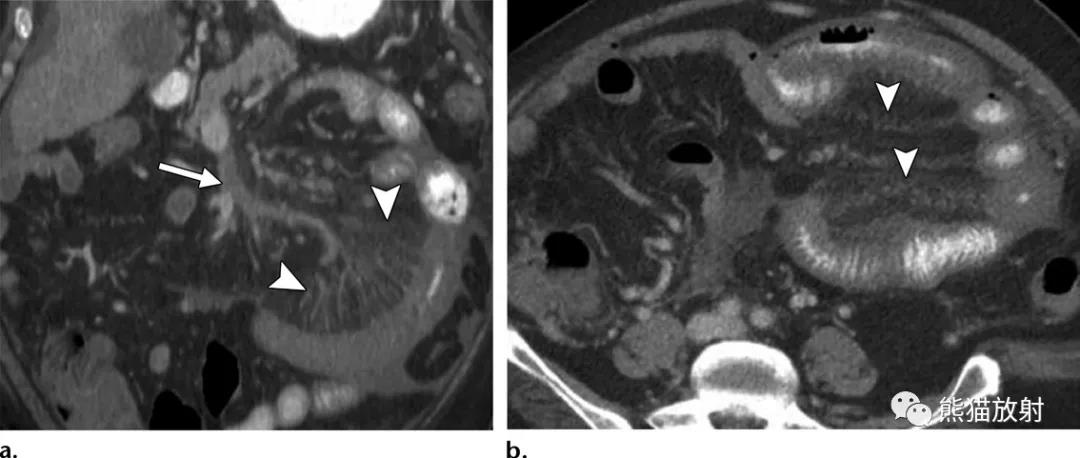
闭环性小肠梗阻(closed-loop small-bowel obstruction)。上图:51岁女性,直肠癌术后,增强CT显示空肠环及其肠系膜血管增生呈放射状,并逐渐汇聚至梗阻中心,呈鸟嘴征。注意缺血段(箭)肠管壁分层呈靶征,并肠系膜水肿,积液和血管充血。下图:43岁女性,复发性小肠梗阻,曾行剖腹探查术,增强CT显示回肠在两个点处被阻塞,呈U形(虚线新月形)闭合袢样结构。
低灌注复合表现
Hypoperfusion Complex
血流灌注不足。30岁男性,发生车祸。增强CT显示部分空肠肠壁增厚,黏膜明显强化(白箭)。下腔静脉塌陷(箭头),主动脉直径缩小(黑箭)和局部水肿,提示灌注不足。
小肠血管炎
Small-Bowel Vasculitides

狼疮血管炎。43岁女性,患有系统性红斑狼疮(SLE),严重腹痛。增强CT显示小肠扩张,弥漫性对称性肠壁增厚,黏膜明显强化。注意末端血管的螺丝锥样表现(箭),这是与基础血管炎有关的小血管缺血性疾病的特征。
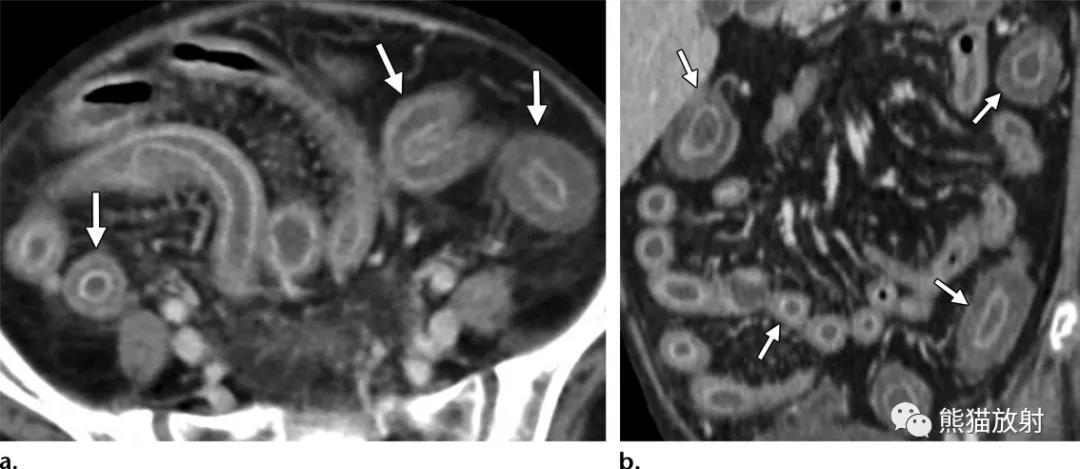
过敏性紫癜(HSP)血管炎。42岁男性,血便。增强CT显示多个空肠壁呈靶征(箭),肠系膜血管充血,腹水。
小肠血管性水肿
Angioedema of the Small Bowel

2名患者,因ACE抑制剂引起的血管性水肿。(a)39岁女性,最近开始增加赖诺普利的剂量,弥漫性腹痛,增强CT图像显示部分空肠水肿,肠壁分层(箭)。(b)47岁女性,接受ACE抑制剂治疗,口腹造影剂和增强CT图像显示小肠壁增厚、分层(箭)。(c)b图同一患者,ACE抑制剂停用后1个月后,CT示出炎性改变完全缓解(*)。
免疫病因所致小肠疾病
Immunologic Causes of Small-Bowel Disorders
移植物抗宿主病
Graft-versus-host disease (GVHD)
29岁女性,急性髓细胞性白血病病史,在接受异体干细胞移植后2年出现了小肠梗阻复发,小肠造影显示了小肠分离(箭),具有典型的“牙膏”或“飘带样”外观,代表了GVHD的长期收缩改变。
21岁女性,髓样肉瘤病史,接受同种异体干细胞移植后73天出现中性白细胞减少,出现GVHD。增强CT显示弥漫性肠壁水肿伴靶征(箭),导致弥漫性肠腔狭窄。内镜活检结果证实类固醇难治性GVHD。
医源性小肠病变:放化疗所致肠炎
Iatrogenic Causes of Small-Bowel Disorders: Radiation Therapy– and Chemotherapy-induced Enteritis
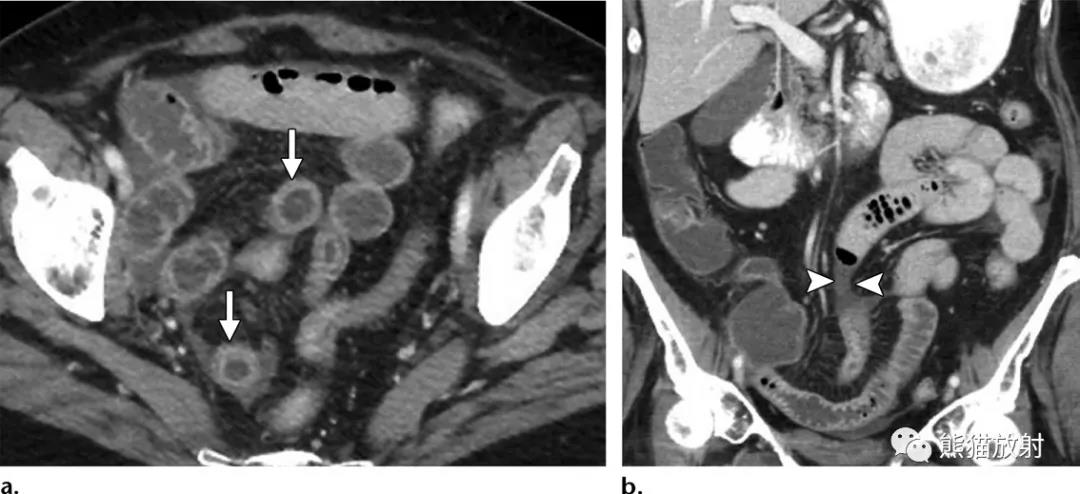
59岁女性,慢性肠病,急性呕吐和腹痛,10年前因宫颈癌接受了化疗和放疗。增强CT显示盆腔部分回肠壁增厚(箭)呈靶征,伴有管腔狭窄(b箭)和由于放射性缩窄而引起的远端小肠梗阻。
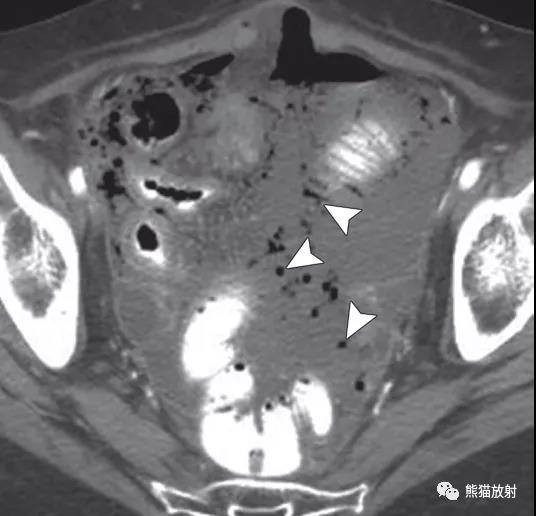
62岁女性,放射性肠炎急性穿孔,宫颈癌放疗后突发剧烈腹痛。增强CT显示回肠壁部分增厚,肠腔积液,盆腔可见腹水和多发斑点状气体(箭),提示小肠穿孔。

66岁,女性,慢性放射性肠炎,患有宫颈癌且曾接受过化疗和放疗,反复出现小肠梗阻。小肠造影显示盆腔部分回肠壁增厚(箭头),呈“堆叠硬币”样外观,局部肠腔狭窄(箭),与慢性放射性肠病有关。

舒尼替尼相关性肠炎。58岁男性,转移性肾细胞癌,表现为腹痛和腹泻。口服造影剂、增强CT图像显示小肠壁增厚(箭头),壁分层,其特征是黏膜和固有肌层明显增强。

贝伐单抗相关性肠炎。58岁转移性直肠癌患者,腹痛和腹泻。增强CT显示部分小肠壁增厚,壁分层(a箭头),小肠静脉充血(b箭头)和局部肠系膜水肿(箭)。
急性小肠穿孔
Acute Small-Bowel Perforation
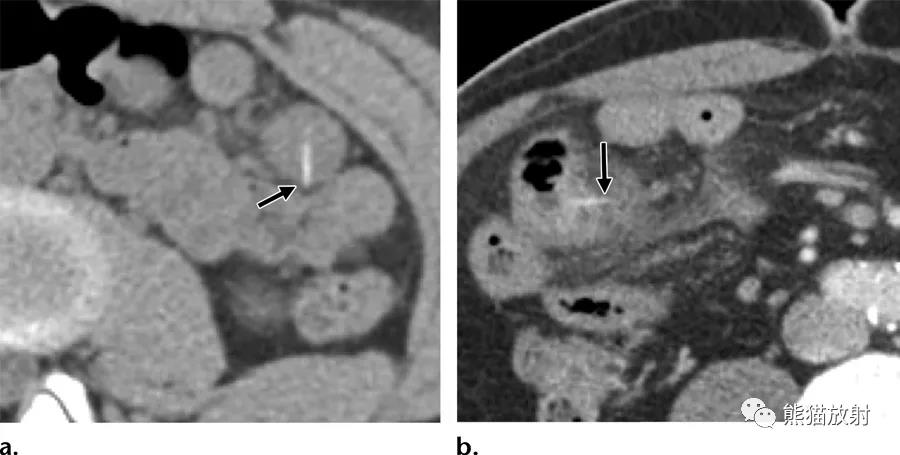
肠异物穿孔。(a)吃下小骨头的16岁女孩,CT平扫显示左中腹部小肠(箭)见线状高密度延伸穿过肠壁,后来手术证实。(b)78岁女性右侧腹痛,增强CT显示细长骨质密度(箭头)引起局灶性小肠穿孔,伴有肠壁水肿,肠系膜脂肪浑浊和腹水。
经手术证实的创伤性空肠穿孔,两名患者均在机动车碰撞后腹痛。(a)24岁男性,增强CT显示空肠壁明显强化伴有肠系膜水肿,肠系膜积液(箭)和腹腔积血。(b)27岁男性,增强CT显示空肠局灶性穿孔,肠壁明显强化(箭头)和肠系膜动脉活动性出血,造影剂外渗(箭头),符合Treitz韧带水平肠系膜损伤。
Crohn 病
Crohn Disease

活动性克罗恩病肠炎。53岁男性,增强CT显示远段回肠节段性肠壁增厚、黏膜明显强化(箭)和上游肠腔扩张(*)。
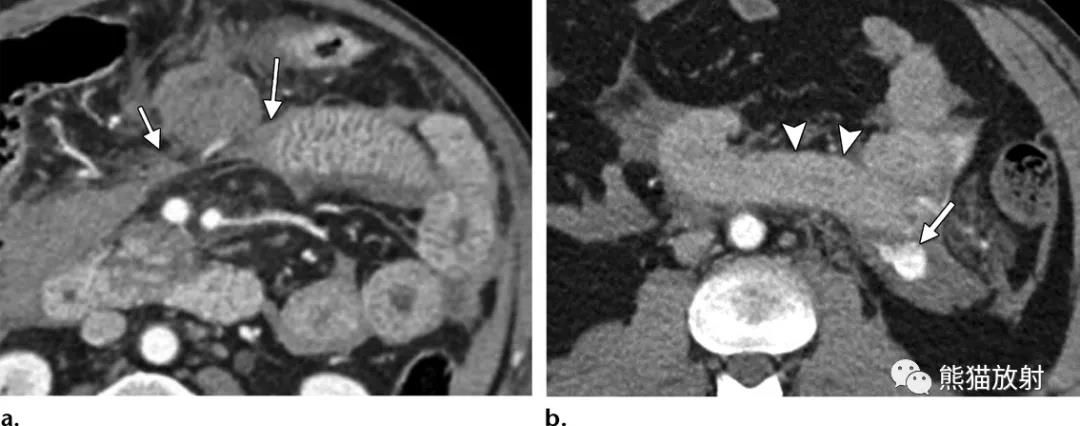
克罗恩病,活动性炎症并伴有肠梗阻。(a)56岁女性,冠状增强CT显示新末端回肠肠壁明显增厚和黏膜明显强化,肠系膜充血呈典型的梳样改变(箭头)。局部明显管腔变窄(*)并上游肠腔扩张,提示活动性克罗恩病。(b)39岁女性,冠状口服造影剂增强CT显示部分肠壁明显增厚并强化,并炎性狭窄(箭)伴上游回肠扩张。
克罗恩病并伴有瘘管形成。68岁男性,冠状增强CT显示星状复杂的小肠-结肠瘘(*),炎性软组织肿块将部分相邻结肠和小肠束缚到一个中心点,受累小肠呈靶征,相应肠系膜水肿。
小肠出血
Hemorrhage in the Small Bowel
(相关内容见下表)
鉴别诊断的关键特征
Identifying Key Features for Differential Diagnosis
急性小肠疾病的临床和CT表现
Clinical and CT Features of Acute Small-Bowel Diseases

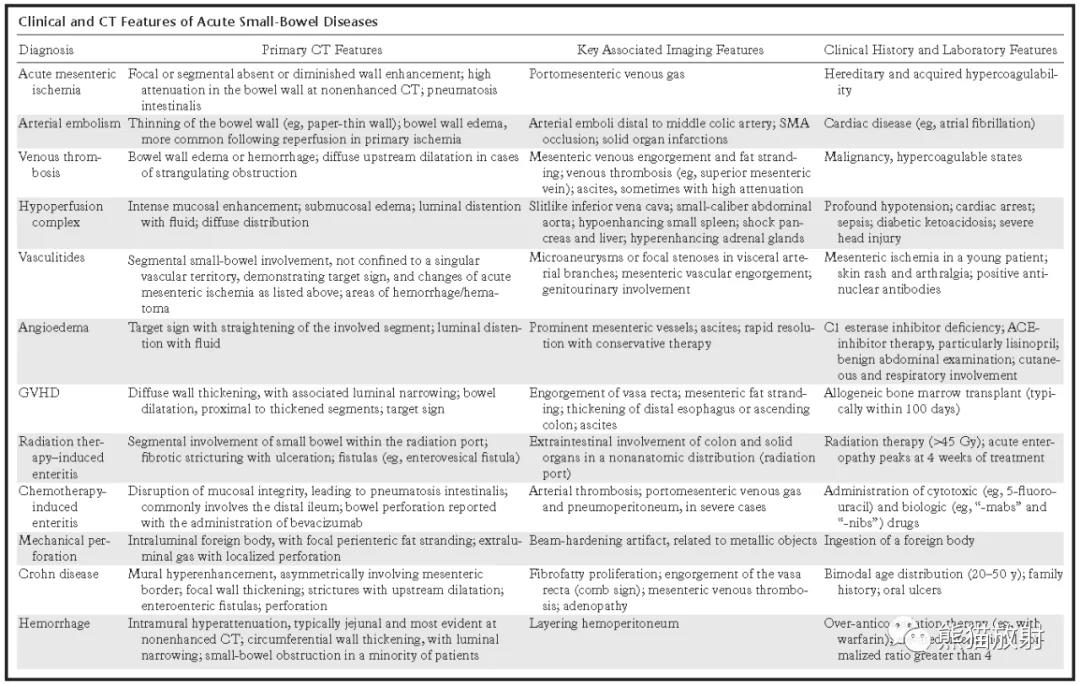
小结
小肠易患多种疾病,表现为与结肠不同的CT表现。急性疾病的影像学特征有很大的重叠,通常首先在CT上进行评估,肠壁环形增厚、分层是最常见的表现。对影响小肠疾病的病理生理学的了解可以帮助寻找第二影像学特征,并将其与可用的临床信息相结合,有助于鉴别诊断。
↓ 以上内容整理自:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
142
学习了 收藏
146
很详细,学习了!
161
学习了
151
好
141
#CT表现#
83