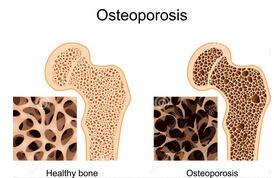
Ann Rheum Dis:骨质疏松性骨折风险预测工具的准确性:系统回顾和荟萃分析
2015-10-22 candy 译 MedSci原创
目的:识别目前可用的预测骨折风险精度的工具的准确性。方法:研究人员系统检索到2014为止的PubMed MEDLINE,EMBASE和Cochrane数据库。两位评阅者独立筛选文献,收集研究数据,对各研究中的参考文献进行手动检索。使用诊断准确性研究的质量评估工具(QUADAS),最主要的结果包括AUC曲线下面积,95%置信区间和ROC曲线分析。研究者排除没有外部验证或专门针对特定疾病人群的预测工具
目的:识别目前可用的预测骨折风险精度的工具的准确性。
方法:研究人员系统检索到2014为止的PubMed MEDLINE,EMBASE和Cochrane数据库。两位评阅者独立筛选文献,收集研究数据,对各研究中的参考文献进行手动检索。使用诊断准确性研究的质量评估工具(QUADAS),最主要的结果包括AUC曲线下面积,95%置信区间和ROC曲线分析。研究者排除没有外部验证或专门针对特定疾病人群的预测工具。对纳入标准的工具进行随机效应荟萃分析。
结果:45项研究符合纳入标准,对应13种不同的预测工具。只有三个工具经过超过一次的以人群为基础的测试。FRAX(9个国家,26个研究),GARVAN(3个国家,6个研究)和QFracture(英国,3个研究,其中1个有爱尔兰研究者的参与)。这三个工具涉及了27个研究,共17个荟萃分析(对髋部或全身骨质疏松性骨折;男性或女性;有无骨密度)。
结论:13种预测工具在临床实践中都是可行的。FRAX拥有最大数量的外部验证和独立研究。不同的工具的整体精度是令人满意的(>0.70),如QFracture达到了0.89(95% CI 0.88 to 0.89)。在许多研究中观察到明显的方法论局限性和风险倾向。仍然需要评估骨折预测工具的校准性的高质量研究。因此,研究者建议预测工具比较时,对于完全基于AUC曲线下面积的做法应谨慎;并建议为了国际无偏倚比较和更好的定量合成,研究人员应该根据需求和适应症使用预测工具。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#准确性#
112
#荟萃分析#
86
#荟萃#
87
这篇文章有一定深度
178
是一篇不错的文章
144
实用
150
不错,赞一个
144
#Dis#
79
真不错
157
#骨质疏松性骨折#
54