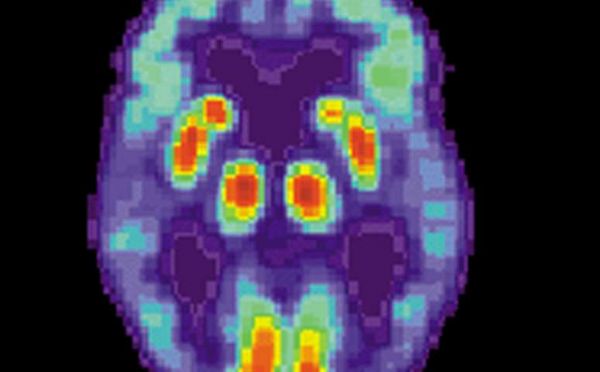
Brain:脑影像学进展确定阿兹海默症传播发展的关键蛋白,老年痴呆有救了
2018-01-08 佚名 medicalxpress
最近在脑成像方面的进展首次表明,在阿尔茨海默氏病中,一种导致神经细胞死亡的关键蛋白在整个大脑中传播,因此阻止它的传播有望阻止这种疾病的蔓延。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#影像学进展#
83
#关键蛋白#
124
学习一下谢谢分享
101
学习了.涨知识
129
#阿兹海默症#
84
好
118
学习了新知识
116
学习学习.继续关注
103