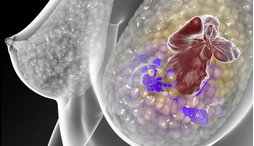
JAMA Surgery:男女性乳腺癌患者接受双侧乳房切除术的利与弊
2015-09-04 MedSci MedSci原创
根据美国癌症协会的调查显示,许多人都没有意识到男性也会患乳腺癌,且他们所占比重为1%。虽然男性乳腺癌患者仅为女性患者的1/100,但2012年美国乳腺外科学会的研究发现,男性乳腺癌患者相比女性而言,生存率更低。女性浸润性乳腺癌患者双侧乳房切除术的比例显著增加,由1998年的2.2%上升至2011年的11%。这一数据引起广大医务人员的关注。去年5月,Medical News Today报道称,发表在
根据美国癌症协会的调查显示,许多人都没有意识到男性也会患乳腺癌,且他们所占比重为1%。虽然男性乳腺癌患者仅为女性患者的1/100,但2012年美国乳腺外科学会的研究发现,男性乳腺癌患者相比女性而言,生存率更低。
女性浸润性乳腺癌患者双侧乳房切除术的比例显著增加,由1998年的2.2%上升至2011年的11%。这一数据引起广大医务人员的关注。
去年5月,Medical News Today报道称,发表在JAMA Surgery的研究称乳腺癌患者接受双侧乳房切除术其实本不必要,因为没有足够证据表明该术式真正有效。最近的一项研究表明,双侧乳房切除术不能降低乳腺癌患者的死亡率。
Ahmedin Jemal和他的同事们开始着手研究接受双侧乳房切除术的男性乳腺癌患者比例是否增高。他们收集了北美中央癌症登记协会(NAACCR)的相关数据,统计了2004-2011年之间共6332名浸润性乳腺癌男性患者的治疗信息和相应数据。
结果显示,在这7年间,接受双乳房切除术的男性患者几乎翻了一番,由2004年的3%上升至2011的5.6%,上升了86.7%。
购有死人医疗保险的年轻白人接受该手术的数目最多,同样条件下的女性患者也较多接受该类型手术。
遗传检测、家族病史、磁共振成像(MRI)、恐惧等因素会影响女性是否接受双侧乳房切除术,但研究人员指出,这些因素是否会影响男性患者接受双侧乳房切除术尚未可知。但是,毫无疑问的是,在接受手术前,医生要与患者合理沟通,根据病情做出全面解释,并尊重患者的决定。
Jemal博士认为,接受双侧乳房切除术患者数目的增加,当不清楚是否可以增加患者的生存率,但是毫无疑问主要目的是为了提高患者的治疗效果和生存质量。
医务人员应该密切关注男性和女性乳腺癌患者的治疗状况,详细告知他们双侧乳房切除术的益处和弊端,以帮助患者做出正确的决定,并能够有利于提高他们的生存质量和治疗效果。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GER#
80
#surgery#
77
#切除术#
73
#双侧#
67
#乳腺癌患者#
62
看到了
116