CLIN CANCER RES:LKB1表达与化疗及贝伐单抗治疗的晚期非小细胞肺癌患者预后改善有关
2017-07-08 MedSci MedSci原创
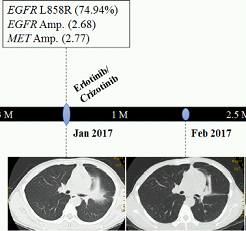
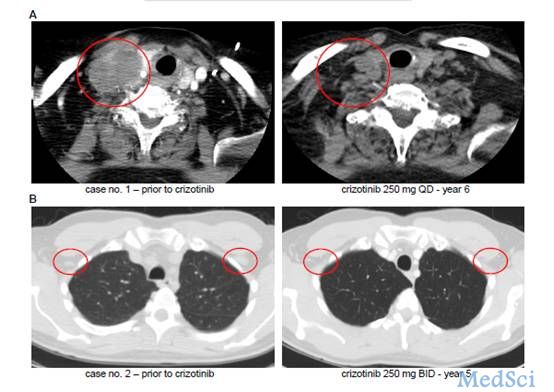
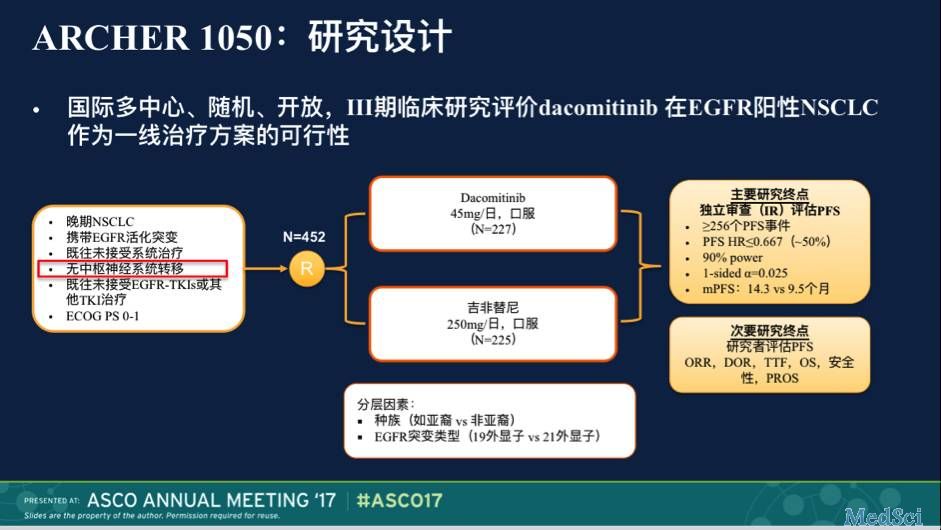
LKB1是包括缺氧、糖剥夺等在内的代谢压力的主要感应物质之一,抗血管生成疗法会加重肿瘤微环境中缺氧及糖剥夺情况。CLIN CANCER RES近期发表了一篇文章,研究LKB1是否可以作为晚期非小细胞肺癌(aNSCLC)贝伐单抗治疗敏感的预测标志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
52
#患者预后#
68
#肺癌患者#
67
抗血管生成药物并不是广谱抗癌药,学习了
68
学习了,谢谢分享
77
#非小细胞肺癌患者#
56
#贝伐#
59
#LKB1#
63
学习一下吧!学习一下了!
63
继续学习中谢谢
86