一、病史简介
女性,46岁,浙江人,2016-06-13入中山医院感染病科
主诉:反复发热伴干咳4月余
现病史:
2016-02 无明显诱因下出现发热,Tmax 39.8℃,伴畏寒、干咳,当地医院予以抗感染、止咳等治疗(具体不详)后体温下降,但咳嗽未能缓解。
2016-04 再次发热,Tmax 40℃,咳嗽症状明显加重,自行服用退热药后体温平,咳嗽好转不明显。
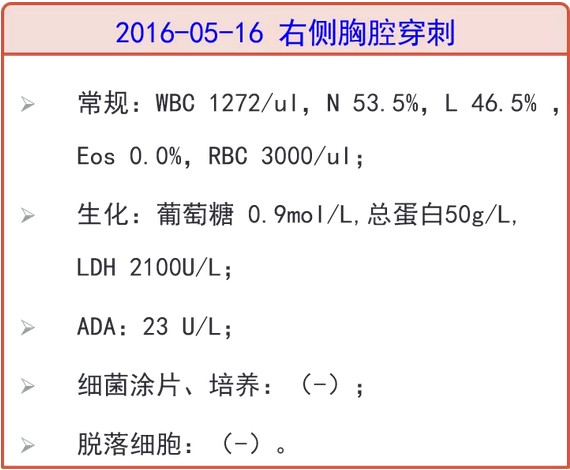
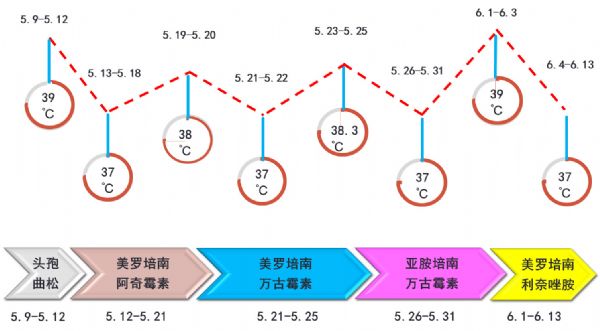
2016-05-07 胸部CT:左肺感染,两侧胸腔、心包积液。05-09当地医院住院治疗,查WBC 4.8*10^9/L、N 70.1%、CRP 19.5mg/L、PCT<0.05ng/ml、血培养(-)、心超(-)。予头孢曲松抗感染,仍高热。
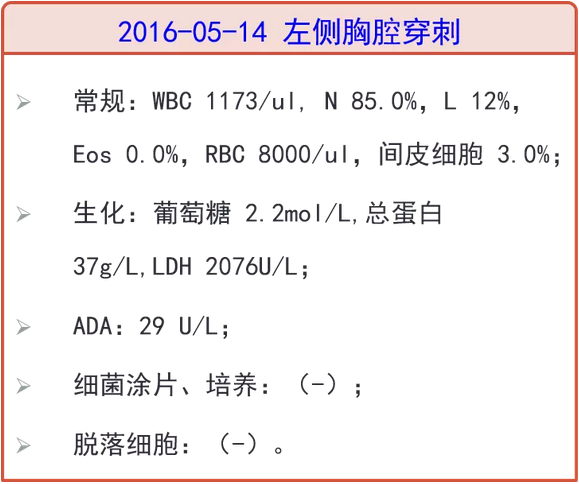
2016-05-12 复查胸部CT:左肺病灶较前进展,胸腔积液较前增多,改美罗培南+阿奇霉素抗感染10天,期间分别行双侧胸腔积液穿刺引流,均提示渗出液,体温下降至正常后又复升至38.0℃。05-13、05-17 复查两次血培养,均(-)。
2016-05-21 来上海中山医院接受专家心超:二尖瓣及主动脉瓣增厚毛糙、主动脉瓣粟米状赘生物形成、少量心包积液。当地医院综合考虑,拟诊感染性心内膜炎,予以万古霉素+美罗培南抗感染,咳嗽较前好转,体温转平,但2天后再次发热,Tmax 38.1℃。05-25查:WBC 6.1*10^9/L、N 84.6%、CRP 35mg/L。
2016-05-26 转至上海某三甲医院,住院期间体温正常,复查胸部CT左上肺病灶基本吸收、双侧少量包裹性胸腔积液,心超未见赘生物。考虑肺部感染,感染性心内膜炎不能除外,予以万古霉素+亚胺培南抗感染3天,无发热,嘱出院。
2016-06-01 Tmax 39℃,伴畏寒,咳嗽不明显,再次至当地医院住院治疗。继续予万古霉素联合美罗培南抗感染,用药期间,患者消化道症状显着,随访Scr进行性升高至192umol/L,考虑万古霉素导致药物性肾损伤,06-02起改予利奈唑胺+美罗培南抗感染,06-04起体温逐渐降至正常,复查上海中山医院专家心超,报告二尖瓣及主动脉瓣增厚毛糙、主动脉瓣粟米状赘生物形成。期间再次复查血培养仍(-)。06-07查血WBC 2.8*10^9/L、N 57.7%、CRP 10.4mg/L、Scr 171umol/L。
为明确诊断和进一步治疗,2016-06-13 拟“发热待查”转上海入住我院感染病科。
既往史:高血压病史1年余,血压最高180-190/90-100mmHg,予口服降压药治疗(具体不详)1年余。
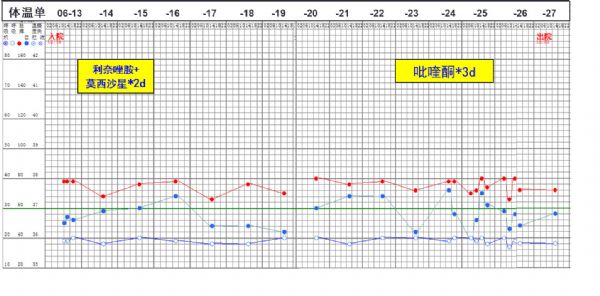
外院治疗期间体温及用药史
二、入院检查(2018-06-13)
体格检查
T 36.5℃,血压144/90mmHg,皮肤黏膜未及淤点,未及Osler结节,两肺未闻及干湿啰音。心前区无隆起,心界不大,心率79次/分,律齐,各瓣膜区未闻及杂音。
实验室检查
血常规: WBC 3.71*109/L,N 69.2%,Eos% 0.02%;炎症标志物:ESR:40 mm/H;CRP:23.4mg/L;PCT 0.07ng/ml;铁蛋白:227.8 ng/ml。
肝肾功能:ALT/AST(-), Alb 34g/L, Cr 133umol/L,IgE 48 U/mL。
肿瘤标志物: CA125 78.9 U/ml, CA153 38.1U/ml,余(-)。
尿常规、粪常规:正常。
细胞免疫:正常。
BNP:197.7 pg/ml,心肌损伤标志物:正常范围;
T-SPOT.TB:0/0; G试验(-);血隐球菌乳胶凝集试验(-);
EBV、CMV-IgG、IgM:(-)
呼吸道九联检:(-);
自身抗体:(-);
血培养:(-);
辅助检查:
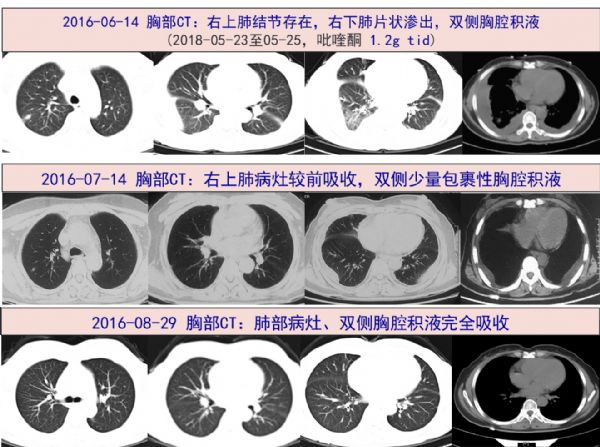
胸部CT:双肺炎症(右肺为着),双侧胸腔积液伴双肺部分膨胀不全。
腹部增强CT:肝血管瘤可能。
心电图:窦性心律,T波改变。
三、临床分析
病史特点:患者中年女性,因反复发热伴干咳4月余,炎症标志物轻度升高,多次胸部CT提示肺内病灶、胸腔积液,肺内病灶为结节、片状渗出,部位不固定,外院胸腔积液检查提示渗出液,ADA 29/23U/L;多次血培养阴性,两次心超提示二尖瓣及主动脉瓣增厚毛糙、主动脉瓣粟米状赘生物形成、少量心包积液。外院予以头孢曲松、美罗培南+阿奇霉素、万古霉素+美罗培南/亚胺培南、利奈唑胺+美罗培南等方案抗感染后仍反复发热,仔细回顾发热及用药史,似每次换药后有所好转,但几日后再次高热,实则无规律可循,因患者除发热外还有肺部、心脏累及可能,需与以下疾病鉴别:
感染性心内膜炎(IE):亚急性起病多见,常发生于伴器质性心脏病患者,链球菌是自体瓣膜IE的常见病原体,主要表现为发热等全身毒性症状和心脏瓣膜区杂音,可伴有菌栓脱落所致的迁徙病灶等。由于抗菌药物的应用,IE临床表现常不典型。该患者反复发热,两次心超提示二尖瓣及主动脉瓣增厚毛糙、主动脉瓣粟米状赘生物,故需考虑该IE,但患者无心脏结构异常、查体瓣膜区未及杂音,多次血培养阴性,多种抗感染方案治疗后均无好转,尤其是患者双侧胸腔积液和心包积液而无心衰表现,不支持IE的诊断。
结核病:患者有反复发热、咳嗽,病程较长,胸部CT示多浆膜腔积液(胸膜腔和心包),并有肺部散在小斑片和纤维病灶,胸腔积液检验显示为渗出液,多种抗菌药物治疗效果不佳,需要考虑肺、胸腔和心包结核。但该患者胸水细胞以中心粒细胞为主,ADA较低(分别为23和29U/L),尤其是T-SPOT.TB为0/0,故本病可能性也不大。
寄生虫病:发热伴双侧胸腔积液和心包积液,肺部小斑片病灶部位似不固定,炎症标志物轻度升高,病程较长,多种强效广谱抗菌药物治疗效果不佳,在感染性疾病中需要考虑之前抗感染治疗不能覆盖的病原体引起的感染包括寄生虫病,可进行血寄生虫抗体、胸水检查等。
风湿性疾病:风湿性疾病如SLE可表现为发热、多浆膜腔积液,少数SLE也可出现心脏瓣膜赘生物,该类赘生物叫Libman-sacks赘疣,也称无菌性心内膜炎,但患者自身抗体均阴性,无SLE其他表现,故暂不考虑。
四、进一步检查、诊治过程和治疗反应
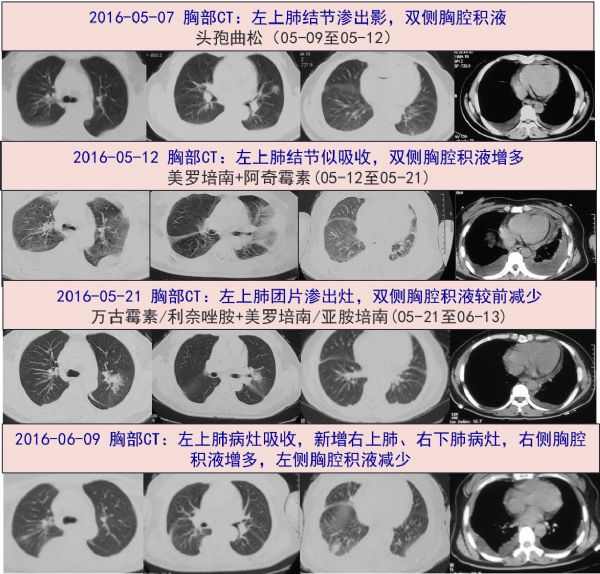
·2016-06-14 考虑肾功能不全,结合之前用药情况,调整抗感染为利奈唑胺 0.6g q12h +莫西沙星 0.4g qd。但用药后恶心呕吐明显,考虑入院后体温平,血培养未报阳性,感染性心内膜炎证据不足,予停抗感染治疗。
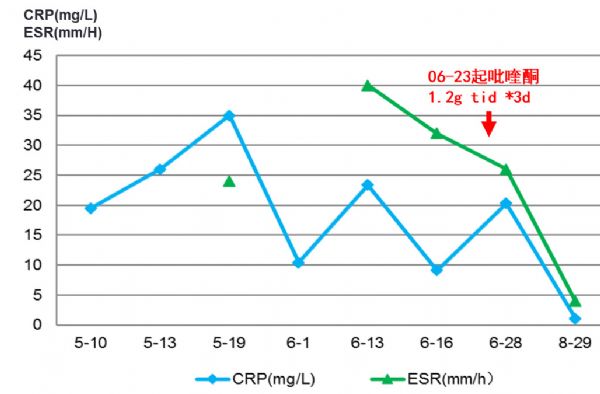
·2016-06-16 复查炎症标志物:ESR:32 mm/H;CRP:9.1 mg/L;
·2016-06-20 主任查房,追问病史患者浙江宁波人,平素喜食醉蟹等,结合外院多次影像学病灶提示游走性斑片影,虽嗜酸性粒细胞、IgE均无升高,寄生虫感染不能除外,抽血外送寄生虫抗体全套。
·2016-06-20、06-22 分别行介入彩超下右侧、左侧胸腔穿刺引流术,引流液均提示渗出液,ADA 48U/L。
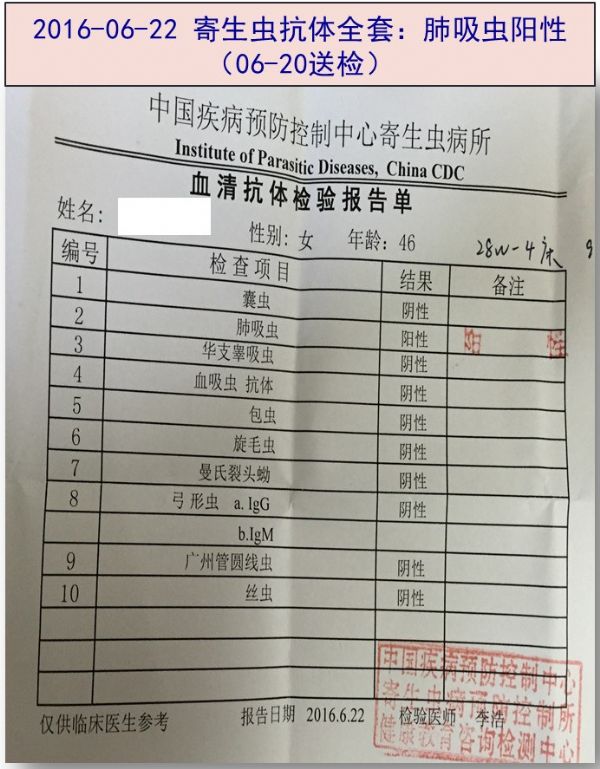
·2016-06-22 寄生虫抗体结果回报:肺吸虫阳性。次日开始予以吡喹酮 1.2g tid*3d抗寄生虫治疗。
·2016-06-27 体温平,咳嗽症状好转,复查炎症标志物ESR:26 mm/H;CRP:20.3 mg/L;肝功能正常。06-28 复查心超:二尖瓣及主动脉瓣增厚毛糙,粟米状赘生物附着,心包未见积液。予以出院。
体温单及用药情况
出院后随访
患者在2016-06-28 出院后,未使用其他药物,自觉进一步好转,无发热,无咳嗽症状。2016-07-14当地胸部CT提示双侧残留少许胸腔积液。
2016-08-29 我院门诊随访,炎症标志物 ESR:8 mm/H;CRP:2.3 mg/L,复查专家心超仍提示二尖瓣及主动脉瓣增厚毛糙、粟米状赘生物(已机化)。
炎症标志物
五、最后诊断与诊断依据
最终诊断:
肺吸虫病
诊断依据:
患者中年女性,反复发热伴干咳4月余,喜食醉蟹,胸部CT示双侧胸腔积液和心包积液,肺内病灶呈小斑片影部位不固定,多种抗菌药物治疗无效,虽然血和胸腔积液嗜酸性细胞不高,但寄生虫抗体显示“肺吸虫阳性”,予吡喹酮治疗后获得显着效果,即未再出现发热和咳嗽,肺内病灶及胸腔积液、心包积液完全吸收,炎症标志物降至正常,故肺吸虫病诊断成立。
患者多次心超均报告为“瓣膜毛糙/粟米状赘生物”,而且之后随访瓣膜变化不大,抗感染效果不佳,血培养多次阴性,所以发热原因不考虑感染性心内膜炎。心瓣膜上述病变,可能是既往感染或其他疾病引起炎症后所残留的陈旧性改变。
六、经验与体会
肺吸虫病,也称并殖吸虫病,以卫氏并殖吸虫和斯氏并殖吸虫引起多见,主要因生吃或半生吃含有肺吸虫囊蚴的第二中间宿主淡水蟹类、蝲蛄所致。急性肺吸虫可表现为发热、腹痛腹泻、胸闷气短、咳嗽等,慢性肺吸虫病主要表现为咳嗽、咳痰、咯血,卫氏并殖吸虫更易导致肺实质病变,影像学可表现为肺结节、实变和囊性病灶;斯氏并殖吸虫更易引起胸膜病变,如气胸、胸腔积液、胸膜增厚等。
肺吸虫病主要依靠显微镜下检查,在感染后8-10周时,部分病例可通过痰液、BAL或粪便中发现特征性的虫卵(卵圆形,棕色,壳较厚,大小约为100μm×55μm)而诊断。血清学检查也可作为肺吸虫病诊断的辅助检查,ELISA法具有较好的敏感性(92%)和特异性(>90%),感染后2-3周即可检测到抗并殖吸虫特定抗体,但方法作为检测患者治疗效果作用有限。值得指出,近十多年来,我国医院检验人员从显微镜下发现特征性虫卵确诊肺吸虫病罕有报告,可能与此病发病率低检验人员形态学检查经验不足、以及病情较轻排卵较少有关,临床确诊病例,绝大多数是根据血清学检查结果的。
本例反复发热4月伴干咳,胸部CT显示双侧胸腔积液和心包积液,肺内病灶呈小斑片影部位不固定,多种抗菌药物治疗无效,是需要考虑肺吸虫可能。然而外周血嗜酸性粒细胞不高,干扰了临床医生对寄生虫病的诊断思路。其实,国际上有文献报道,至少有20%的肺吸虫不出现嗜酸性粒细胞升高和/或IgE升高,所以对于临床表现高度提示但外周血甚至胸水中嗜酸性粒细胞不高者,临床医生仍需对寄生虫感染的警惕性。本例便是基于这个理念,我们及时做血寄生虫抗体检测,终于让发热长达4个月的病人获得了正确的病原学诊断和针对性抗感染治疗。
原始出处:
[1]Brahmer JR, et al. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018 Jun10;36(17):1714-1768.
[2]Seon HJ , et al. Differential Chest Computed Tomography Findings ofPulmonary Parasite Infestation Between the Paragonimiasis and NonparagonimiaticParasite Infestation. J Comput Assist Tomogr. 2015 Nov-Dec;39(6):956-61.
[3]Nagayasu, E., et al. Paragonimiasis in Japan: a twelve-yearretrospective case review (2001-2012). Intern Med, 2015. 54(2): p. 179-86.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好极了,值得分享。
107
好病例,复杂病历,简单原因,看到最后有种柳暗花明之感
111
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
105
嗯嗯,学习学习。
111
好好好好好好好好
0
学习了感谢分享
45