Cell:抗病毒“新兵”打造人体**道防线 新机制为抗艾药物研发提供新途径
2019-01-25 辛雨 中国科学报
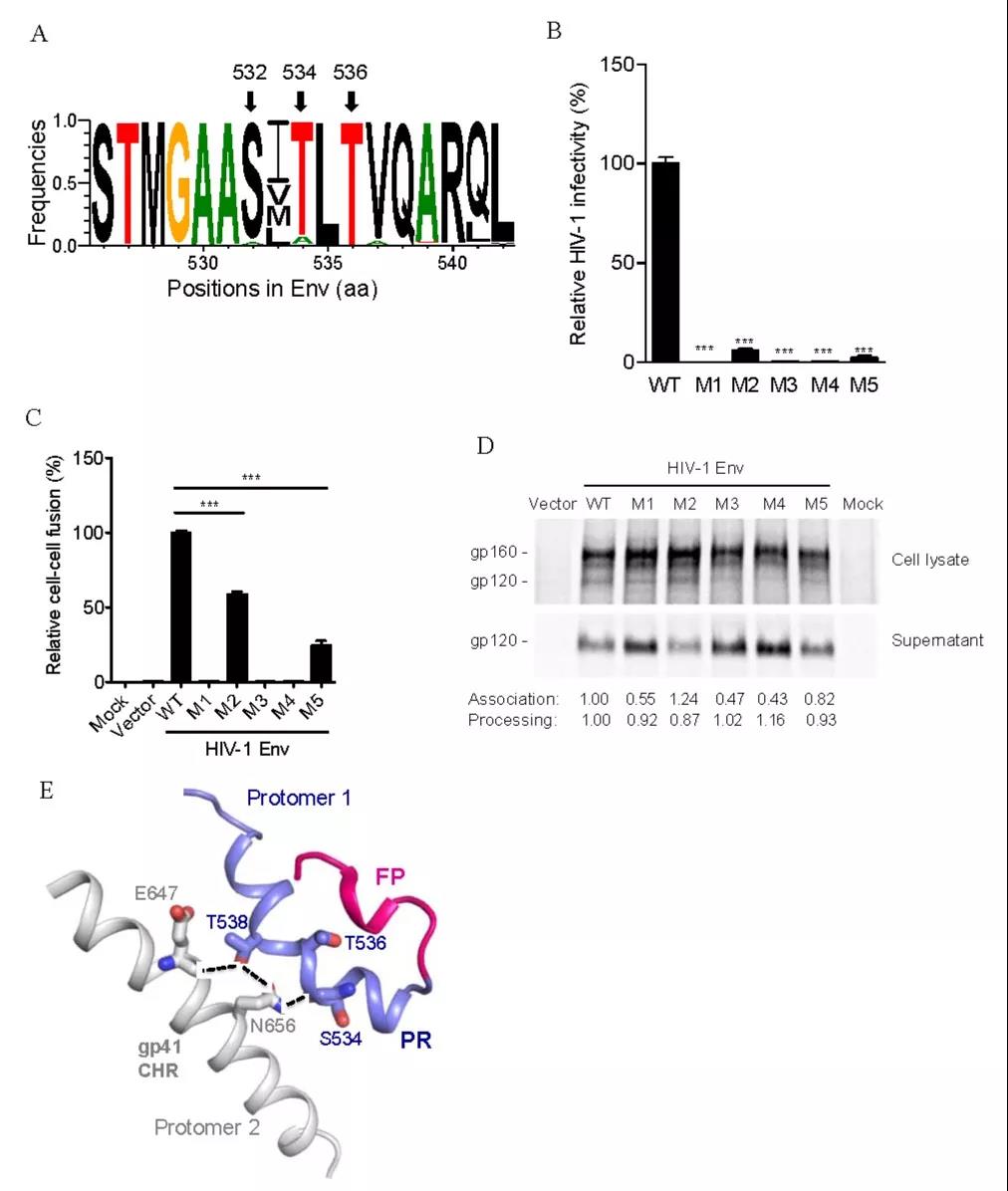
1月24日,中国科学院生物物理所研究员高光侠团队在《细胞》发表研究称,首次发现了新的宿主抗病毒因子,可抑制人类免疫缺陷病毒1型(HIV-1)蛋白质翻译过程中的程序性-1位核糖体移码,从而抑制病毒在细胞内复制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新途径#
85
#Cell#
65
#CEL#
55
#抗病毒#
69
#研发#
66
#药物研发#
62