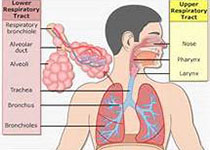
Chest:阿托伐他汀治疗铜绿假单胞菌感染的支气管扩张患者疗效如何?
2017-06-03 xing.T MedSci原创
由此可见,该研究结果表明阿托伐他汀可以降低感染铜绿假单胞菌的支气管扩张患者全身炎症和改善生活质量。这些效应可能是由于阿托伐他汀调节中性粒细胞活化能力所致。
在重症支气管扩张、慢性铜绿假单胞菌感染的患者中,尚没有采用他汀类药物治疗的随机对照试验(RCT)。
近日,呼吸领域权威杂志chest上发表了一篇研究文章,研究人员将32例慢性铜绿假单胞菌感染患者招募入双盲交叉RCT中。每个队列中招募了16例患者,分别给予80mg阿托伐他汀或安慰剂治疗3个月,接下来进行6周的洗脱期,进行交叉并给予替代治疗3个月。
共有27例患者完成了研究治疗 。阿托伐他汀没有明显改善通过莱斯特咳嗽问卷测量的咳嗽这一主要终点[平均差异为1.92,95%可信区间为(-0.57至4.41),P=0.12]。然而,阿托伐他汀治疗可改善圣乔治呼吸疾病问卷(-5.62分,P=0.016),降低血清CXCL8(P=0.04)、肿瘤坏死因子(P=0.01)和细胞间粘附分子-1(P=0.04)的水平。具有改善血清CRP与血清中性粒细胞计数(分别有P=0.07和P=0.06)的趋势。在体外实验中,研究人员发现10μM的阿托伐他汀可以减少fMLF诱导的CD11b表达上调和反映降低中性粒细胞激活能力降低的钙流变化。
由此可见,该研究结果表明阿托伐他汀可以降低感染铜绿假单胞菌的支气管扩张患者全身炎症和改善生活质量。这些效应可能是由于阿托伐他汀调节中性粒细胞活化能力所致。
原始出处:
Pallavi Bedi,et al. A randomised control trial of atorvastatin in bronchiectasis patients infected with Pseudomonas aeruginosa- a proof of concept study.chest.2017. http://journal.publications.chestnet.org/article.aspx?articleid=2630498
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EST#
47
#Chest#
50
#支气管#
54
#扩张#
60
真是大开眼界啦!
130
还阿托伐他汀钙还有这种作用,对它的药理作用需要再看看
92
学习了,提高了
93
学习啦谢谢分享
94
非常好的文章,学习了,很受益
107
一药多用,非常好
77