急性肺栓塞是急诊科比较常见的凶险疾病之一,也是常见的三大致死性心血管疾病之一。肺血栓栓塞症是由来自静脉系统或右心的血栓阻塞肺动脉或其分支所致,以肺循环和呼吸功能障碍为主要病理生理特征和临床表现,通常所说的急性肺栓塞即指肺血栓栓塞症。中华医学会急诊医学分会等组织发表了中国急性血栓性疾病抗栓治疗共识,下面整理其中有关急性肺栓塞抗凝与溶栓治疗部分的内容,与大家分享。 1 危险分层 根据患者的血流动力学及肺栓塞严重指数(PESI)将急性肺栓塞的早期死亡风险分为高危、中危、低危。出现休克或持续性低血压者为高危;对不伴休克或持续性低血压的非高危患者,根据PESI或简化版PESI,区分中危和低危。根据是否有右室功能障碍及心肌损伤生物标记物异常,将中危者再分为中高危或中低危。 2 抗凝治疗 急性肺栓塞的抗栓治疗包括抗凝、溶栓、经皮导管介入治疗及外科血栓清除术,目的是恢复闭塞肺动脉的血流,挽救生命,或预防潜在致命性栓塞再发。 (1)所有明确诊断为急性肺栓塞(亚段肺栓塞除外),且无抗凝禁忌者,立即开始抗凝治疗(IC)。 (2)对高度或中度急性肺栓塞临床可能性者,在等待诊断结果的同时给予抗凝治疗(IC)。 (3)亚段肺栓塞,且无下肢近端深静脉血栓(DVT)者,伴静脉血栓栓塞症(VTE)再发低风险者,建议临床观察(IIC);对亚段肺栓塞伴VTE再发高风险者,建议抗凝治疗(IIC)。 (1)对高危肺栓塞患者,推荐立即静脉给予普通肝素抗凝(IC)。 (2)对大多数中低危肺栓塞患者,推荐LMWH或磺达肝癸钠抗凝(IA)。 (3)对大多数中低危肺栓塞患者,可以采用达比加群(150 mg每天两次,对80岁以上或使用维拉帕米者,剂量110 mg每天两次),替代VKA治疗,联合胃肠外抗凝(IB)。 (4)对大多数中低危肺栓塞患者,可以采用利伐沙班(15 mg每天两次,持续治疗3周后改为20 mg每天一次),替代胃肠外抗凝序贯VKA治疗(IB)。 (5)对有严重肾功能不全的肺栓塞患者,不推荐DOAC(IIIA)。 (6)对肺栓塞不合并恶性肿瘤,且适合DOAC者,长期(3个月)抗凝可以使用达比加群、利伐沙班(IIB)。 (7)对肺栓塞合并恶性肿瘤者,可以采用LMWH作为长期抗凝药(IIC)。 首先给予负荷剂量2000~5000 IU或80 IU/kg普通肝素静脉注射,继之以18 IU/kg/h持续静脉滴注。在初始24小时内需每4~6小时测定一次活化的部分凝血酶原时间(APTT),根据APTT调整普通肝素的剂量,每次调整剂量后3小时再测定一次APTT,使其尽快达到并维持在正常值的1.5~2.5倍。治疗达到稳定水平后,改为每天测定一次APTT。 应用普通肝素可能引起HIT,在使用第3~5天必须复查血小板数量。如果需要较长时间使用普通肝素,要在第7~10天、第14天复查血小板计数。普通肝素使用2周后,较少出现HIT。 LMWH按体重给药,无需监测,在孕期应定期监测Xa因子活性。 对大多数中低危肺栓塞患者,可以考虑达比加群或利伐沙班作为替代方案。其中利伐沙班不需要提前肝素化,可立即使用,或在胃肠外抗凝治疗1~2天后开始使用,但需在前3周增加剂量。在使用达比加群作为替代方案时,需提前使用胃肠外抗凝药。 (2)对无明显诱因的首发肺栓塞,伴低-中出血风险者,推荐延长抗凝治疗(无预期抗凝终点)(IIB);伴高出血风险者,推荐3个月抗凝治疗(IB)。 (3)对无明显诱因的复发肺栓塞,伴低出血风险者,推荐延长抗凝治疗(无预期抗凝终点)(IB);伴中度出血风险者,推荐延长抗凝治疗(无预期抗凝终点)(IIB);伴高出血风险者,推荐3个月抗凝治疗(IIB)。 (4)对肺栓塞伴恶性肿瘤者,推荐延长抗凝治疗(无预期抗凝终点)(对非高危出血者,IB;对高危出血者,IIB)。 3 溶栓治疗 中高危肺栓塞患者是否需要溶栓治疗一直存在争议。在患者出现血流动力学不稳定或休克之前,早期发现和逆转右室功能障碍对治疗至关重要,溶栓可以迅速改善右室功能和肺灌注,但增加出血风险。 (2)对没有休克或低血压的肺栓塞者,不推荐常规全身溶栓治疗(IIIB)。 (3)对中高危的急性肺栓塞患者严密监测,及时发现血流动力学失代偿,及时行再灌注治疗(IB)。 (4)对中高危、有血流动力学障碍临床征象的肺栓塞患者,推荐溶栓治疗(IIaB)。 出血性卒中;3~6个月缺血性卒中;已知的结构性脑血管病(如动静脉畸形)或颅内恶性肿瘤;近3周内重大外伤、手术或头部外伤;疑似主动脉夹层;1个月内消化道出血;已知的高出血风险。 4 经皮导管介入治疗 (1)对存在全身溶栓禁忌或全身溶栓治疗失败的肺栓塞患者,考虑经皮导管介入治疗作为外科血栓清除术的替代方案(IIaC)。 (2)如果溶栓治疗的出血预期风险很高,可考虑中高危者行经皮导管介入治疗(IIbB)。 5 外科血栓清除术 (1)外科血栓清除术适用于存在溶栓治疗禁忌,或全身溶栓治疗失败的高危肺栓塞者(IC)。 (2)如果溶栓治疗的出血预期风险很高,可考虑中高危者行外科血栓清除术(IIbC)。 来 源:中国急救医学2019年第39卷第6期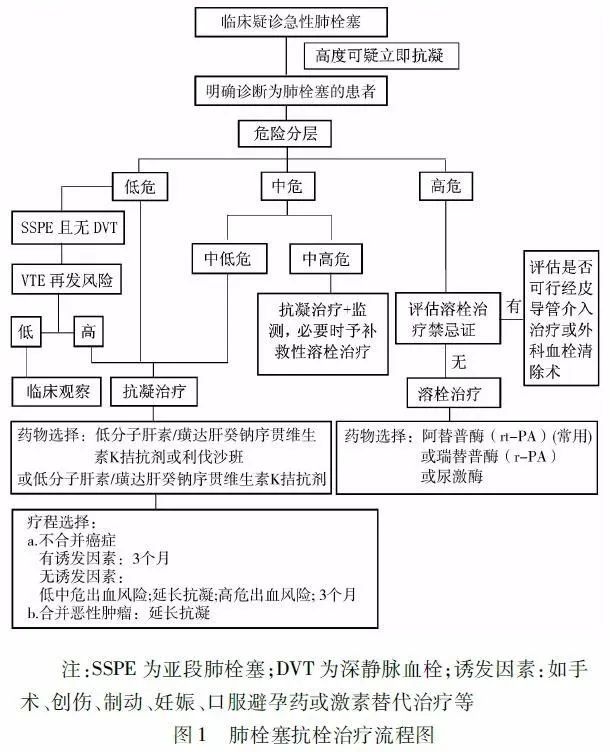
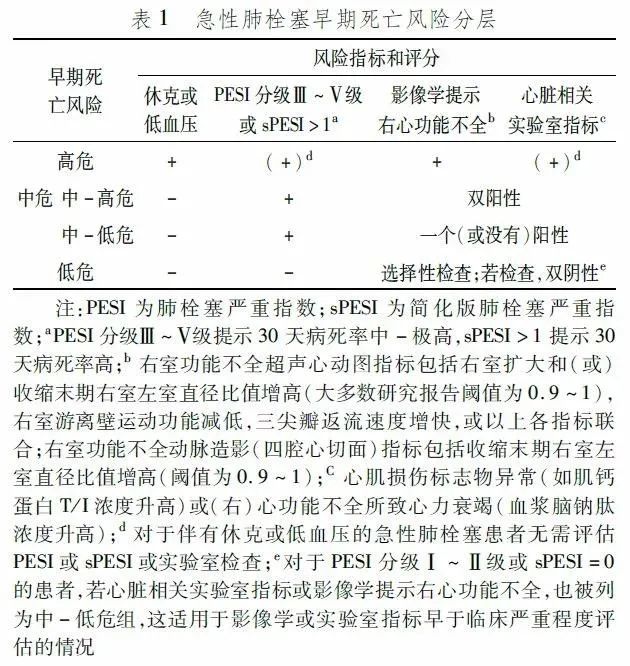
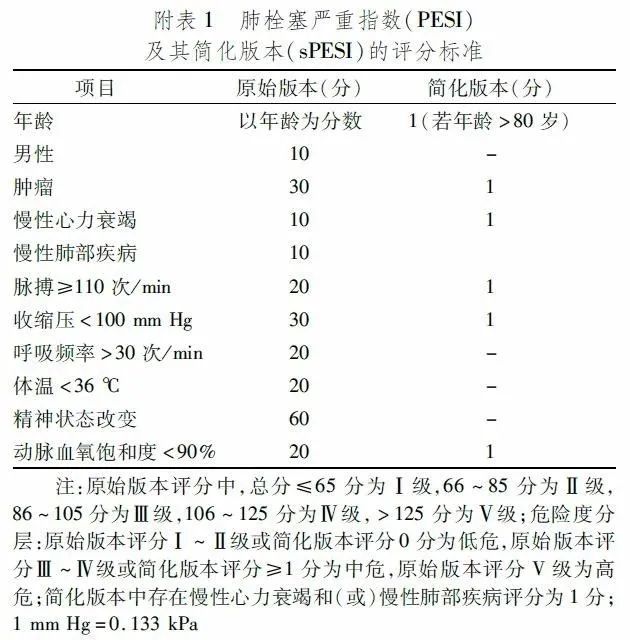
1. 抗凝适应证
2. 抗凝药物
目前临床常用的抗凝药包括胃肠外抗凝药(普通肝素、低分子量肝素LMWH、磺达肝癸钠)、传统口服抗凝药维生素K拮抗剂(VKA),以及新型的直接口服抗凝药(DOAC)。共识对抗凝药物的推荐如下。
3. 抗凝药用法
在初始抗凝治疗中,LMWH、磺达肝癸钠抗凝的效果优于普通肝素,发生大出血、肝素诱导血小板减少症(HIT)的风险较低。普通肝素具有半衰期短、可迅速被鱼精蛋白中和的优点,推荐用于拟行直接再灌注及严重肾功能不全(肌酐清除率<30 ml/min),或重度肥胖患者。
(1)普通肝素
(2)LMWH
(3)磺达肝癸钠
体重不到50 kg者,磺达肝癸钠抗5 mg每天一次;体重50~100 kg者,7.5 mg每天一次;体重超过100 kg者,10 mg每天一次。
(4)VKA
华法林的初始剂量为1~3 mg,一些患者如老年、肝功能受损、慢性心衰及高出血风险者,初始剂量还可以适当减低。应尽早给予口服抗凝药,最好与胃肠外抗凝药同日,通常需重叠治疗5天以上;当INR达到目标范围(2~3)并维持2天以上,可停用普通肝素、LMWH或磺达肝癸钠。
(5)DOAC
4. 抗凝疗程
(1)对有明显诱发因素(如手术、创伤、制动、妊娠、口服避孕药或激素替代治疗等)的急性肺栓塞患者,建议抗凝治疗3个月,优于短程抗凝(3个月以内)(IB)、长程抗凝(如6、12、24个月)(IB)、延长抗凝(无预期抗凝终点)(IB)。
1. 溶栓适应证
(1)对高危肺栓塞者,推荐溶栓治疗(IB)。
2. 溶栓禁忌证
(1)绝对禁忌证
(2)相对禁忌证
年龄≥75岁;6个月内短暂性脑缺血发作(TIA);应用口服抗凝药;妊娠或分娩后1周;不能压迫止血部位的血管穿刺;近期曾行心肺复苏;难以控制的高血压(收缩压超180 mmHg或舒张压超110 mmHg);严重肝功能不全;感染性心内膜炎;活动性溃疡。对危及生命的高危急性肺栓塞患者,大多数禁忌证应视为相对禁忌证。
3. 溶栓方案
我国常用的溶栓药物有尿激酶、阿替普酶(rt-PA)、瑞替普酶(r-PA)。目前我国医院多采用rt-PA,标准剂量100 mg,在2小时内静脉滴注。部分研究表明,与标准剂量rt-PA相比,低剂量的有效性和安全性更好,尤其是体重低于65 kg、右心功能障碍者获益更多。对于rt-PA剂量,共识推荐50~100 mg持续静脉滴注2小时;体重低于65 kg者,总剂量不超过1.5 mg/kg。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












认真学习
96
#急性肺栓塞#
95
努力学习
103
学习#学习#
122
很有用,收藏了
122
挺好的,学习了
105