基础科研:Omicron感染者流行病学研究发表,揭示了真实世界中的病情严重程度
2021-12-22 生物探索 网络
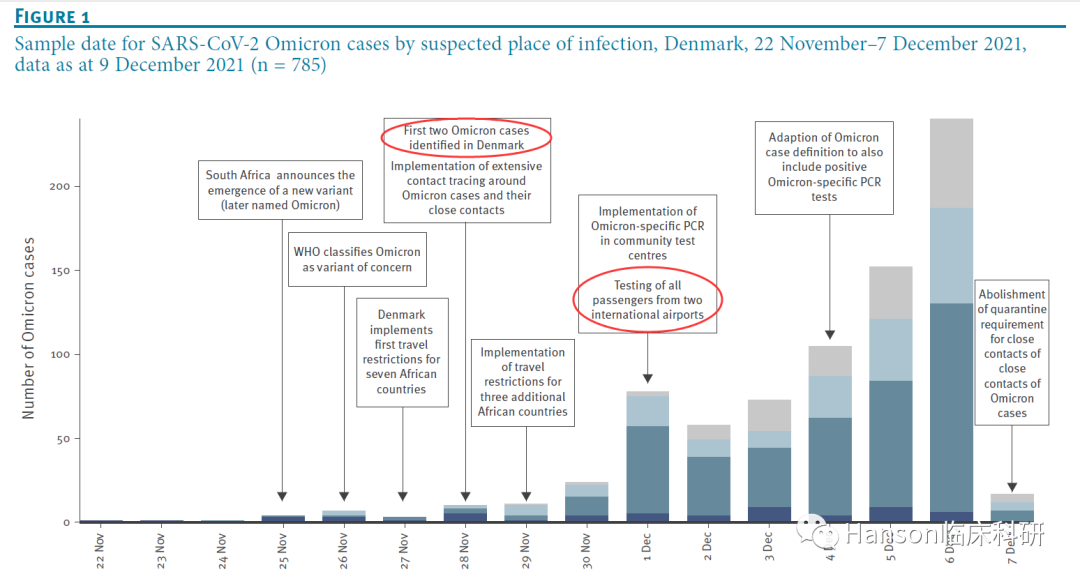
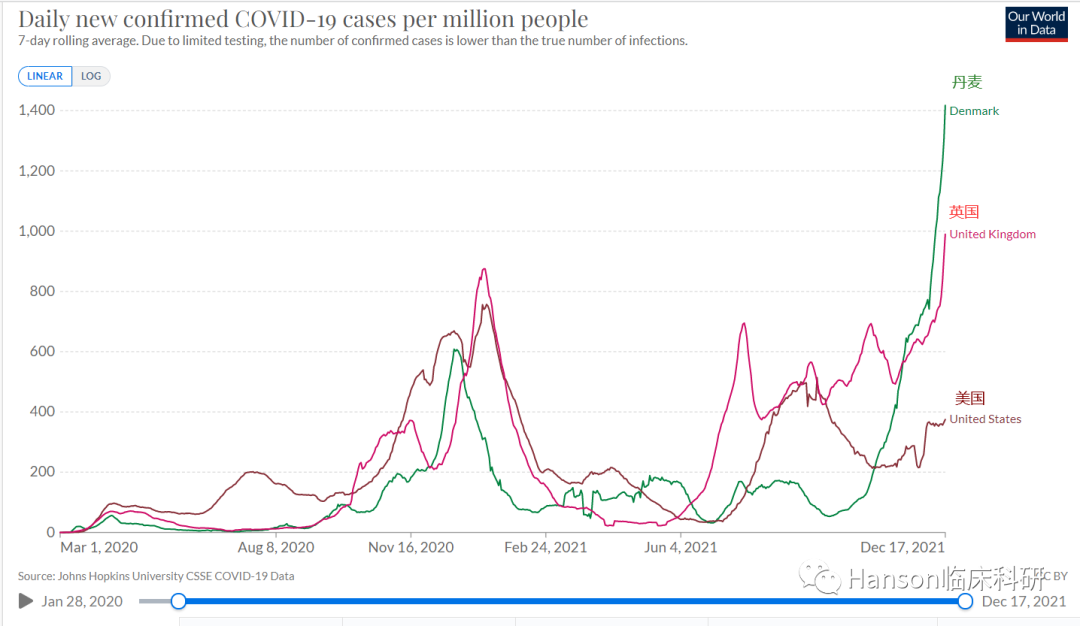
丹麦的研究显示,该国Omicron病例从12月4日开始,每天增长40%。这意味着不到两天就翻一番。
本文转载自“Hanson临床科研”微信公众号。


End
参考资料:
[1]https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.50.2101146#html_fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CRO#
66
#病情#
80
#基础科研#
67
#Micro#
44
#真实世界#
66
#流行病#
75