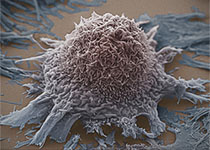
Sci Immunol:研究发现“绞杀”癌症的有效抗体!
2017-05-20 sunshine2015 来宝网
在研究多发性硬化症的基础时,布里格姆和妇女医院的调查人员发现了如何治疗癌症的重要线索。在科学免疫学杂志上发表的一篇文章中,由神经病学家霍华德·韦纳(MD)博士领导的一组研究人员描述了一种可以精确靶向调节性T细胞的抗体,从而释放免疫系统以杀死癌细胞。该小组报告说抗体在黑色素瘤,胶质母细胞瘤和结肠直肠癌模型中降低肿瘤生长,成为癌症免疫治疗的有吸引力的候选者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究发现#
69
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
100
学习了,谢谢分享
119
学习了谢谢分享。
112
学习了,不错
93
学习并分享!!!
75
除了研究其治疗效果之外,我们还想描述抗LAP抗体可以激活免疫系统的机制
101
阅读了谢谢分享。
51
谢谢梅斯医学,受教了
72
谢谢分享,学习了
81