NEJM:体内异物---腹膜游离体
2015-04-07 陈说 译 MedSci原创
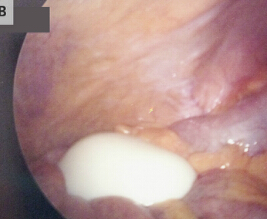
一名患有20年尿频史的65岁男性患者到医院就诊,在体格检查和实验室检查中,均没有发现异常。然而,在计算机断层扫描技术(简称CT)中发现在其腹部和盆腔里存在一个8.5cm的中央已钙化的肿瘤(A图,红色箭头处)向膀胱侧压迫(A图,蓝色箭头处)。通过腹腔镜探查可见,该肿块呈游离状态,表面光滑,质硬,类似于橡胶样的物质,体积为10cmX9.5cmX7.5cm,重220g。(如图B和图C
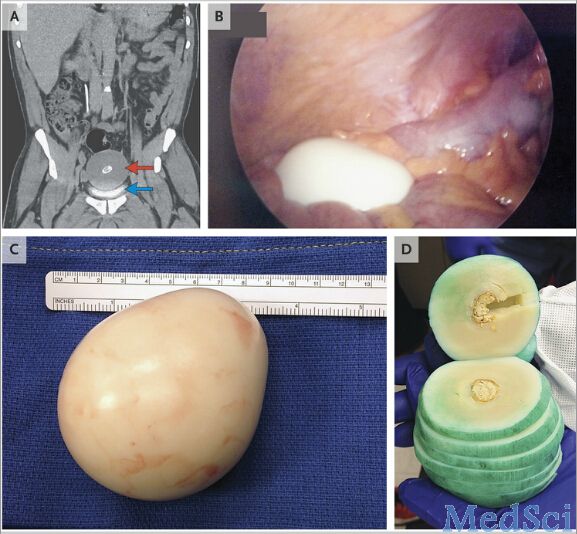
该标本内部分为几层,我们绿色墨水染色将其区分开来。在组织学上来看,其外周大部分的组织是由脱细胞、层压和纤维组织构成;而中间部分主要由蛋白质和纤维素构成,其周围还包裹着一层钙化的物质。经过研究发现,该肿块是一种腹膜游离体。其由腹腔体内的游离纤维物质不断地滚转、坏死,最后形成分离开来的网膜附着物肿块。
起初,这种肿块往往不会引起任何的症状,在其逐渐变大的过程中,相当一部分的病患会出现肠梗阻和尿潴留等症状。如此案例中的病患由于肿块外在的压迫,最后导致了尿频症状。对于这种情况,只需要经手术去除肿块,尿频症状即可得到解决。
腹膜游离体:
一般认为是由于肠脂垂病变扭转、急性炎症、粘连及脱落等原因引起。或者因为慢性炎症刺激引起腹膜间皮增生而形成。由于腹腔内游离物形成机理的复杂性.因此临床上对腹腔内游离物缺乏明确的诊断依据。目前临床上对此病的治疗通常选择手术去除。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
86
舍利子?
145
大千世界,无奇不有
153
像个茶叶蛋一样啊
136
#腹膜#
70
来源是什么?
185
腹膜来源?
104
纤维素坏死物
98
渗出的主要来源是?
125