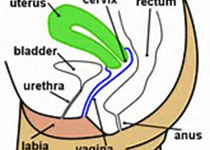
J CLIN ONCOL: Pembrolizumab治疗晚期程序性死亡因子配体 1-阳性的子宫内膜癌的安全及抗肿瘤活性(KEYNOTE-028)
2017-06-21 许奕晗 MedSci原创
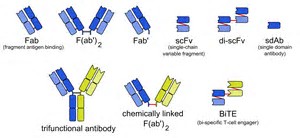
多队列Ib期KEYNOTE-028研究的目的是评估pembrolizumab--一种抗程序性死亡因子 1的单克隆抗体,在程序性死亡因子配体 1(PD-L1)-阳性的晚期实体瘤患者中的安全和疗效。本文报告了晚期子宫内膜癌队列的研究结果。
研究目的:
多队列Ib期KEYNOTE-028研究的目的是评估pembrolizumab--一种抗程序性死亡因子 1的单克隆抗体,在程序性死亡因子配体 1(PD-L1)-阳性的晚期实体瘤患者中的安全和疗效。本文报告了晚期子宫内膜癌队列的研究结果。
患者和方法:
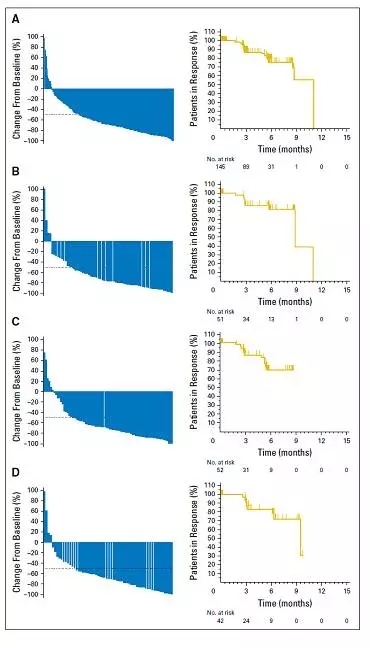
合乎条件的是经历标准治疗后再次进展的局部晚期或者转移的PD-L1-阳性的女性患者。患者接受pembrolizumab 每两周10mg/kg,共计24个月或者至疾病进展或不可接受的毒性反应。主要的疗效终点是 RECIST (1.1版) 提供的客观应答率。次要终点包括安全性、反应持续时间(DOR)、无进展生存期和总体生存期。数据截止日期是2016年2月17日。
研究结果:
筛选出的75例患者中,36例(48.0%)有PD-L1-阳性的肿瘤,24例(32.0%)纳入研究。这24例患者中有15人(62.5%)之前至少接受了两项晚期疾病的治疗。3例患者(13.0%)达到了部分缓解(95% CI,2.8%至33.6%),尚未达到中位DOR。2例患者仍在接受治疗,并在数据截止时表现出持续的反应。另有3例(13.0%)病情稳定,中位持续时间为24.6周。1例获得部分缓解的病人有聚合酶E突变。13例患者(54.2%)出现了与治疗相关的不良事件(AE):疲劳(20.8%)、皮肤瘙痒(16.7%)、发热(12.5%)、食欲下降(12.5%),且在≥10%的患者中发生。4例患者出现了3级与治疗相关的AEs。没有患者发生4级AE,而且没有病人因为AE而终止治疗。
结论:
在预处理过的晚期PD-L1-阳性的子宫内膜癌患者的亚组中,Pembrolizumab显示出良好的安全性和持续的抗肿瘤活性。
原始出处:
Patrick A.Ott. et al.Safety and Antitumor Activity of Pembrolizumab in Advanced Programmed Death Ligand 1-Positive Endometrial Cancer: Results From the KEYNOTE-028 Study. J CLIN ONCOL.2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
87
#抗肿瘤活性#
76
#mAb#
85
#KEYNOTE#
92
#PE#
88
#程序性死亡#
84
#肿瘤活性#
91
#内膜#
74
#Pembro#
77
了解了解
103