盘点:2016多发性骨髓瘤指南及知名杂志研究汇总
2016-08-26 MedSci MedSci原创
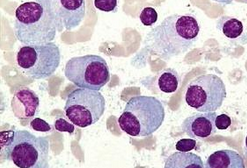
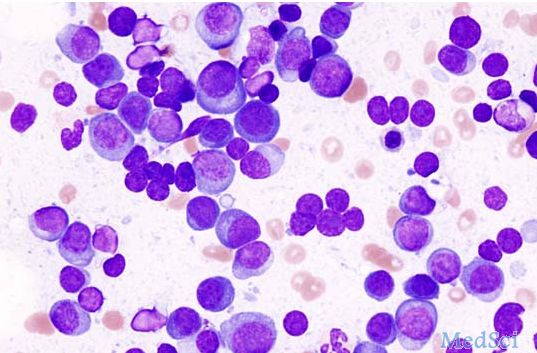
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里小M整理了2016年以来关于多发性骨髓瘤的研究新进展与各位一同分
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里小M整理了今年以来关于多发性骨髓瘤的指南及重要研究新进展与各位一同分享。
【1】 Daratumumab、硼替佐米和地塞米松联合治疗多发性骨髓瘤效果更好
近日,发表于NEJM的一项新的研究发现表明,在复发或难治性多发性骨髓瘤患者中,daratumumab联合硼替佐米和地塞米松治疗比单独的硼替佐米和地塞米松治疗有显著更长的无进展生存期,但比硼替佐米和地塞米松单独治疗有更多地输注相关反应,并且发生血小板减少症和中性粒细胞减少几率也更高。
在这项3期临床试验中,研究人员随机分配498例复发或复发难治性多发性骨髓瘤患者接受单独硼替佐米和单独地塞米松,或与daratumumab联合使用。
结果,预先指定的中期分析显示,daratumumab组的无进展生存率显著高于对照组;在12个月时,daratumumab组的无进展生存率为60.7%,对照组为26.9%。在平均随访7.4个月后,daratumumab组的平均无进展生存期未达到,而对照组为7.2个月。 daratumumab组的总体反应率比对照组高,并且daratumumab组非常好或更好的部分缓解率和完全或更好的缓解率都比对照组高。daratumumab组和对照组最常见的3或4级不良事件为血小板减少症,贫血和中性粒细胞减少。在daratumumab组中有45.3%的患者报告了与daratumumab治疗有关的输注相关反应;这些反应大多为1级或2级,并且这些患者中98.2%的患者在第一次输注时就发生了反应。(文章详见——NEJM:Daratumumab、硼替佐米和地塞米松联合治疗多发性骨髓瘤效果更好)

【2】 来那度胺+地塞米松——不适宜移植骨髓瘤患者的治疗新标准
最近,发表于Journal of Clinical Oncology上的一项3期FIRST试验表明,与美法仑、强的松和沙利度胺(MPT)相比,来那度胺+低剂量地塞米松(Rd)的连续治疗明显降低了未经治、且不适宜移植的多发性骨髓瘤(MM)患者的进展风险。
该研究纳入了1623名未经治的症状性MM患者。患者随机接受了来那度胺+低剂量地塞米松治疗直至疾病进展(Rd连续疗法;n = 535)或相同方案持续治疗72周(Rd18;n = 541)或MPT治疗(n = 547)。主要终点是无进展生存期(PFS)。该研究中共35名患者年龄≥75岁。
结果,与MPT治疗组的患者相比,Rd连续治疗组的患者有一个更长的PFS,进展或死亡风险降低了31%。在所有患者中,年龄≤75岁的患者的进展风险降低了36%,而年龄>75岁的患者降低了20%。Rd18组的随访结果与MPT组相似。另外,Rd持续组的总生存期明显改善,中位总生存期比MPT组延长了10个月,并且这种改善在年龄>75岁的患者中更显著。(文章详见——JCO:来那度胺+地塞米松——不适宜移植骨髓瘤患者的治疗新标准)
【3】 强生多发性骨髓瘤药物Darzalex+来那度胺+地塞米松三联疗法III期临床显著延长无进展生存期
美国医药巨头强生(JNJ)在第21届欧洲血液学协会(EHA2016)大会上公布了多发性骨髓瘤药物Darzalex III期MMY3003(POLLEX)临床研究的积极数据。
该研究是一项随机、开放标签、多国、多中心、对照III期研究,在569例既往已接受至少一种疗法的多发性骨髓瘤(MM)患者中开展。数据显示,与标准护理方案lenalidomide+地塞米松二联疗法(Rd)相比,Darzalex+来那度胺+地塞米松的三联疗法(DRd)使疾病进展或死亡风险显著降低63%。中位随访13.5个月的数据显示,Rd二联治疗组中位无进展生存期(PFS)为18.4个月,DRd三联治疗组中位PFS尚未达到,同时总缓解率显著提高。
除了达到改善无进展生存期的主要终点以及显著提高总缓解率之外,与Rd二联治疗组相比,DRd三联治疗组实现完全缓解率(CR)或更好缓解的患者比例显著提高2倍(43% vs 19%,p<0.0001),实现极佳部分缓解(VGPR)或更好缓解的患者比例也显著提高(76% vs 44%,p<0.0001)。
该研究中,DRd三联疗法的安全性与Darzalex(D)单药疗法及Rd二联疗法的安全性一致。该研究表明,在既往已接受治疗的多发性骨髓瘤(MM)群体中,Darzalex联合标准护理可诱导深度缓解,这些激动人心的数据突出了Darzalex作为一种背景治疗方案在既往已接受一线或多线治疗的MM群体中的潜在临床受益。(文章详见——EHA 2016:强生多发性骨髓瘤药物Darzalex+来那度胺+地塞米松三联疗法III期临床显著延长无进展生存期)
【4】来那度胺维持疗法或可明显改善多发性骨髓瘤患者的存活率
此前有很多研究发现,在自体造血干细胞移植后进行来那度胺维持治疗或可改善新诊断多发性骨髓瘤患者的总体生存率,而其它多发性骨髓瘤患者却并未因此获益,相关研究发表于近日举办的2016年美国临床肿瘤学会年会上。
这项研究中,研究者对CALGB、IFM及GIMEMA进行的三项随机对照试验进行综合分析,研究包括1200多名参与者;其中有605名新诊断的多发性骨髓瘤患者,这些患者在自体造血干细胞移植后进行来那度胺维持治疗,同时对照为604名接受安慰剂或不进行维持治疗的患者,7年后研究者发现,进行来那度胺维持治疗的患者中有62%的患者存活着,而对照组中有50%的患者存活着,同时患者总体生存率在各研究组中基本一致。(文章详见——ASCO 2016:来那度胺维持疗法或可明显改善多发性骨髓瘤患者的存活率)
【5】T细胞受体疗法(TCR)治疗骨髓瘤疗效良好
1/2期试验结果显示,对于多发性骨髓瘤患者,自体干细胞移植之后进行新型T细胞受体(TCR)疗法治疗是安全的,而且与临床缓解和无进展生存期改善相关。文章发表在Nature Medicine上,Lancet Oncology配发了评论。
研究人员评估了自体T细胞设计表达亲和力增强的TCR的安全性和有效性,它可以识别肿瘤-睾丸抗体NYESO-1和LAGE-1共享的缩氨酸。大约60%的晚期骨髓瘤患者表达NY-ESO-1。20名显示抗体阳性的多发性骨髓瘤患者接受自体干细胞移植2天后,接受平均2.4 × 10⁹的工程T细胞输注。T细胞输注耐受性良好,尽管白介素6浓度较高,但是没有出现明显的临床细胞因子释放综合征。
治疗之后中位随访21.1个月,10/20名患者仍然无进展生存,15名患者存活,5名死亡。治疗后的100天,14名患者发生接近完全缓解或完全缓解。中位无进展生存期为19.1个月的16名患者发生良好的临床缓解。(文章详见——Nat Med:T细胞受体疗法(TCR)治疗骨髓瘤疗效良好)

【6】Ixazomib、来那度胺、地塞米松治疗可显著延长多发性骨髓瘤患者的无进展生存期
发表于NEJM的一项研究表明,将ixazomib加入到来那度胺和地塞米松方案中可显著延长无进展生存期;与口服疗法相关的毒性作用也是有限的。
在此双盲、安慰剂对照、3期试验中,研究人员随机分配722例患有复发性,难治性或复发和难治多发性骨髓瘤患者接受ixazomib加来那度胺-地塞米松(ixazomib组)或安慰剂加来那度胺-地塞米松(安慰剂组)。主要终点是无进展生存期。
在平均14.7个月的随访期间,ixazomib组的无进展生存期显著长于安慰剂组;在所有预先确定的患者亚组中,与安慰剂治疗方案相比,ixazomib治疗都有益于患者的无进展生存期,包括高危细胞遗传学异常的患者。 ixazomib组的总反应率为78%,安慰剂组为72%,相应的完全缓解加上非常好的部分缓解率则分别为48%和39%。ixazomib组的中位反应时间是1.1个月,而安慰剂组为1.9个月,相对应的反应持续中位时间为20.5个月和15.0个月。
在大约23个月的中位随访时,任一研究组的中位总生存期都还尚未达到,而后续随访工作正在进行中。死亡率和严重不良事件的发生率在两个研究组是相似的;至少3级得严重不良事件分别为74%和69%。ixazomib组的3级和4级严重性血小板减少事件比安慰剂组发生更频繁。ixazomib组皮疹的发生率比安慰剂组更频繁,胃肠道不良事件,主要是低级的,在ixazomib组发生更频繁。周围神经病变的发病率在ixazomib组和安慰剂组中分别为27%和22%。在两个研究组患者报告的生活质量是相似的。(文章详见——NEJM:口服Ixazomib、来那度胺、地塞米松治疗可显著延长多发性骨髓瘤患者的无进展生存期(TOURMALINE-MM1研究))
【7】研究鉴别出多发性骨髓瘤的新型治疗靶点
来自美国西奈山伊坎医学院的研究人员通过研究表示,靶向作用CDK4和ARK5两种维持细胞内能量平衡的关键蛋白,就可以有效促进骨髓瘤细胞死亡,相关研究为鉴别新型治疗多发性骨髓瘤的药物提供了新的线索,该研究刊登于Cancer Research杂志上。
研究者同Onconova公司进行合作开发了一种名为ON123300的化合物,其包括有针对ARK5和CDK4的靶向抑制剂,研究者利用该抑制剂处理原发性的骨髓瘤细胞和骨髓瘤细胞系,结果发现该抑制剂可导致肿瘤细胞死亡,从而在体外和体内的动物模型中均可以有效遏制癌症发展。
本文研究揭示了ARK5连接mTOR与MYC通路的新型功能。研究者检测了ARK5/CDK4的抑制剂ON123300在抵御骨髓瘤细胞系及来自骨髓瘤复发患者机体样本上的效应,结果显示,骨髓瘤细胞对ON123300比较敏感,而且正常的外周血细胞可以免于该化合物的影响,这就再次证明了抑制剂ON123300的特殊抗癌潜力;该研究发现抑制剂ON123300可以诱导多发性骨髓瘤细胞死亡,并且可以负向调节关键的致癌通路。(文章详见——Cancer Res:鉴别出多发性骨髓瘤的新型治疗靶点)
【8】高脂联素水平可能会降低肥胖或超重人群的骨髓瘤患病风险
发表于Cancer Research是的一项研究表明,高脂联素水平可能会降低肥胖或超重人群的骨髓瘤患病风险。
在该项研究中,高脂联素水平显著降低了后续患多发性骨髓瘤的风险。之前相关表明,肥胖可增加多发性骨髓瘤患病风险,并且有关研究也表明脂联素水平的降低可能也是风险因素之一。
该研究纳入624例骨髓瘤患者和1246例配对的对照患者。血涂片分析显示,肥胖患者体内的脂联素水平要低于体重正常者,并且该激素水平在对照病例中会随着年龄的增加而增加。
研究人员发现,脂联素最高水平患者与最低水平患者相比,骨髓瘤风险明显降低了36%。研究人员根据身体质量指数对患者进行了分层,并且发现在肥胖和超重患者中,脂联素水平和骨髓瘤风险呈负相关。脂联素水平较高的肥胖或超重患者的骨髓瘤风险明显更低;而在正常体重的患者中,未发现这样的关系。(文章详见——脂联素水平与多发性骨髓瘤有何关系?)
【9】Lancet:Daratumumab治疗难治性多发性骨髓瘤效果显著
发表于NEJM的一项研究daratumumab,一种新的CD38靶向单克隆抗体,对难治性多发性骨髓瘤患者的效果,结果显示Daratumumab单一疗法对于之前治疗过和难治性的多发性骨髓瘤患者在很大程度上显示出令人鼓舞的功效,并且在这一患者群中有良好的安全性。
这项开放性、多中心2期临床试验纳入多发性骨髓瘤患者,以前接受过至少三线疗法治疗或对于蛋白酶抑制剂和免疫调节药物都是难治性的,这些患者在该研究的第1阶段第1部分中被随机以1:1的比例分配接受静脉daratumumab 8mg/kg或16mg/kg,以此来决定第2部分中进一步评估的剂量。患者接受每4周8mg/kg,或16mg/kg,连续8周(1和2周期),然后每2周以此进行16周(3-6周期),然后每4周进行以此(7周期或更高)。在第1部分第2阶段和第2部分中,患者按照第1部分第1阶段接受剂量为16mg/kg。
在该研究第1部分的第1阶段中,18例患者被随机分配到8 mg/kg组,16例患者被分配至16mg/kg组。在第1和2部分中,共有106例接受daratumumab 16mg/kg的患者报告了调查结果。85例(80%)患者曾接受自体干细胞移植,101例(95%)患者对于最近使用的蛋白酶抑制剂和免疫调节药物是难治性的,103例(97%)患者在最后一次治疗中是难治性的。总体响应发生在31例患者中—3例有严格的CR,10例患者有一个非常良好的PR,18例患者有PR。
中位时间到第一次反应的时间是1.0月。缓解时间中位数为7.4个月,无进展生存期为3.7个月。12个月的总生存率为64.8%,在随后的截止阶段,中位总生存期为17.5个月。 Daratumumab的耐受性良好;任何等级的疲劳和贫血是最常见的不良事件。无药物相关的不良事件导致治疗中断。(文章详见——Lancet:Daratumumab治疗难治性多发性骨髓瘤效果显著)
【10】NCCN临床实践指南修订:多发性骨髓瘤(2016.V3)


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
70
好文章,好样的
91
很好,不错,以后会多学习
112
了解一下
86
有意义的指南
86
路过看看
91
值的分享!
67
继续学习
54
继续关注
52